Presentation
A 30-year-old female patient with systemic lupus erythematosus (SLE) was admitted to the hospital because of a three-day history of protrusion of her right eye and mild right eye pain. There were no other visual complaints. She described polyarthralgia and fatigue. She was six months postpartum, and her pregnancy was without any complication.
She had been diagnosed with lupus three years earlier, and her condition had been well controlled with prednisone and hydroxychloroquine. The patient had stopped taking prednisone following the delivery of her baby.
The physical examination revealed the patient’s temperature was 36.4°C (97.6°F), blood pressure was 130/80 mmHg, pulse rate was
85/min and respiration rate was 18/min. The eye examination showed right eye proptosis, and, apart from slight limitation of upward gaze, there was no limitation of eye movement. The small joints of both hands and her left knee were tender and swollen, and there was trace bilateral ankle edema. There was no skin rash or mouth ulcers. The remainder of the examination was normal.
The erythrocyte sedimentation rate (ESR) was 90 mm/hr. The hemoglobin was 12 g/dL, total white cell count was 3,500/mm3 and the platelet count was 252,000/mm3. Urine analysis disclosed 2+ protein; 1+ blood; 2–3 leukocytes, 3–5 erythrocytes/high-power field. Urine protein-creatinine ratio was 1.2 mg/dL, albumin was 3.1 g/dL, and the liver enzymes were normal. Serology tests revealed a positive antinuclear antibody (titer of 1:640) and double-stranded DNA 130 IU/mlL (normal <25 IU/mL). The serum anticardiolipin IgM, IgG and lupus anticoagulant were all negative. Serum complement (C3 and C4) levels were decreased. C3 was 65 mg/dL (normal 88–206 mg/dL), and the C4 was 10 mg/dL (normal range 13–75 mg/dL). Blood cultures and thyroid function tests were normal.
A renal biopsy revealed World Health Organization class III lupus nephritis.
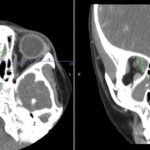
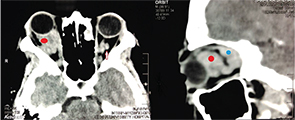
A contrast-enhanced computed tomographic (CT) scan of her orbits was consistent with bilateral orbital pseudotumor with more prominent changes on the right (see Figure 1, above). Proptosis due to pseudo-orbital tumor was considered a part of a lupus flare, and pulse steroids in the form of intravenous methylprednisolone (1 gm) were given daily for three days, followed by high-dose oral prednisone at 1 mg/kg/day.
There was dramatic improvement of the eye swelling, arthralgias, leukopenia and proteinuria. The patient has been in remission with a treatment regimen including mycophenolate mofetil (2 gm/day), hydroxychloroquine (400 mg/day) and low-dose prednisone (10 mg/day).
Discussion
The eye is frequently involved in SLE, with the most common manifestation being keratoconjunctivitis sicca. Other less common causes include cotton wool exudates due to retinal vasculitis, episcleritis and scleritis.
Rarely, the orbit can be affected.1 Orbital disease in patients with rheumatic disease may include primary inflammation of the orbital tissue (e.g., orbital pseudotumor or orbital inflammatory syndrome), inflammation of the extraocular muscles (e.g., orbital myositis), cavernous sinus thrombosis, retrobulbar hematoma, orbital cellulitis, Graves disease or contiguous spread of inflammation from the sinuses, which most typically occurs in ANCA-associated granulomatous vasculitis.2
The most common sign of orbital disease is proptosis caused by a space-occupying lesion or inflammatory process. Associated symptoms and signs include pain, blurred vision, diplopia (double vision) as a result of limitation of eye movement, eyelid swelling and displacement of the globe.3
Orbital pseudotumor, part of the spectrum of idiopathic orbital inflammation, is a nongranulomatous inflammatory disorder that may affect any structure in the orbit. It’s defined according to the orbital structures affected, with the presenting symptoms reflecting the degree of inflammation and the location of the inflamed tissue.4
There are several other reports of SLE presenting with proptosis due to orbital pseudotumor have been published.1,5,6
Patients with an acute presentation may complain of generalized malaise, in addition to ocular symptoms, but are generally afebrile; infections, such as orbital cellulitis, can mimic the features of orbital pseudotumor and should be excluded in patients with pyrexia.5
The diagnosis can be confirmed using CT or magnetic resonance imaging (MRI). In some cases, CT is preferred because of the inherent contrast by different attenuation values of the orbital fat, muscle, bony structures and air in the adjacent paranasal sinuses. Extraorbital extension is better delineated on MRI.
Systemic corticosteroids and immunosuppressive therapy aim to control the underlying disease and can decrease proptosis, improve visual acuity and ocular mobility, and reduce the associated symptoms. Rarely, orbital decompression may be necessary if the inflammatory process has caused proptosis severe enough to compromise the optic nerve (orbital apex syndrome).2
Proptosis in SLE patients represents a diagnostic dilemma, as well as a therapeutic challenge. As our case demonstrates, SLE should be considered in the differential diagnosis of orbital pseudotumor.
Waleed A. Hassan, MD, is a lecturer of rheumatology at Benha University Hospital in Qalubiya, Egypt.
Samy A. Abdelnaby, MSc, is a fellow of ophthalmology at Benha University Hospital in Qalubiya, Egypt.
Yasser M. Abdelhady, MSc, is assistant lecturer of radiology at Benha University Hospital in Qalubiya, Egypt.
References
- McDonald E, Marino C, Cimponeriu D. Painful ophthalmoplegia in a patient with SLE. Hosp Pract. 1992; 27:41–42.
- Watkins AS, Kempen JH, Choi D, et al. Ocular disease in patients with ANCA-positive vasculitis. J Ocul Biol Dis Infor. 2009;3:12–19.
- Bullen CL, Liesegang TJ, McDonald TJ, et al. Ocular complications of ANCA-associated granulomatous vasculitis. Ophthalmology. 1983;90:279–290.
- Weber AL, Romo LV, Sabates NR. Pseudotumour of the orbit. Clinical, pathologic and radiologic evaluation. Radiol Clin North Am. 1999;37:151–168.
- Siebert S, Srinivasan U. Proptosis can be the presenting feature of systemic lupus erythematosus. Ann Rheum Dis. 2004;63:908–909.
- Grimson BS, Simons KB. Orbital inflammation, myositis, and systemic lupus erythematosus. Arch Ophthalmol. 1983;101:736–738.