
Other Clinical Features
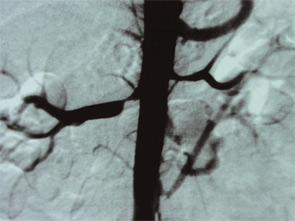
Gastroenterology: As well as Budd-Chiari syndrome—of which APS is a major cause—more focal hepatic thrombosis is frequent, and abnormal liver function tests are frequent in poorly controlled APS. Idiopathic cirrhosis has also been reported in some patients. Celiac axis arterial stenotic lesions were first fully appreciated in angiographic studies of renal artery stenosis. The classical symptoms of post-prandial mesenteric angina were present in most—though not all—of the patients.
Skin: Livedo reticularis is not only an important marker for APS; it could well be a risk factor in itself. Patients with sero-negative APS—as described below—include some with florid livedo. Thrombosis—particularly DVT and skin vessel thrombosis—leads to skin ulceration. For those who conduct skin ulcer clinics, it is clear that a subset of patients exists in whom chronic skin ulceration could well be improved with anticoagulation.
Ear, nose, and throat: My own practice has seen a sharp increase in the number of patients referred by otolaryngologist colleagues, with APS presenting as acute Ménierè’s and balance problems, as well as the well-documented acute sensory neural hearing loss. Tinnitus is a frequently overlooked complaint and I have previously reported the anecdotal experience of tinnitus in APS improving with anticoagulation.
Blood: Severe thrombocytopenia is fortunately unusual, though borderline platelet counts (e.g., 100,000 to 120,000) are frequent. A possible diagnostic clue is the frequency of pseudothrombocytopenia on automatic ethylenediaminetetraacetic acid blood counts (improving on visual counts). This finding possibly points toward subtle platelet membrane abnormalities.
Orthopedics: My colleagues and I have reported a series of idiopathic metatarsal fractures in APS patients, and case reports of other bone fractures (seemingly unrelated to osteoporosis) have appeared. Perhaps the biggest impact in the world of orthopedics will come from more routine screening for prothrombotic conditions prior to hip or knee surgery.12
Pregnancy and in vitro fertilization: The improvement in pregnancy outcome in aPL-positive women during the past two decades has arguably been the headline story of APS and is reviewed elsewhere.13,14 The role of aPL in the pathogenesis of in vitro fertilization (IVF) implantation failure, among other findings, has led to the use of heparin and aspirin in some IVF regimes, though as yet there is little convincing evidence of benefit.

