MADRID—During the 2019 European Congress of Rheumatology (EULAR), June 12–15, researchers reported the results of the ORAL Shift study. This study was a global Phase 3b/4 study of methotrexate withdrawal in rheumatoid arthritis (RA) patients with moderate to severe disease (N=694) who had inadequate responses to methotrexate monotherapy. It was designed as a 12-month randomized, double-blind, placebo-controlled, non-inferiority study.1
MADRID—During the 2019 European Congress of Rheumatology (EULAR), June 12–15, researchers reported the results of the ORAL Shift study. This study was a global Phase 3b/4 study of methotrexate withdrawal in rheumatoid arthritis (RA) patients with moderate to severe disease (N=694) who had inadequate responses to methotrexate monotherapy. It was designed as a 12-month randomized, double-blind, placebo-controlled, non-inferiority study.1
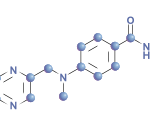
Patients began the study taking 11 mg of open label, extended-release tofacitinib with methotrexate for 24 weeks. Patients who achieved low disease activity with a Clinical Disease Activity Index (CDAI) score of less than 10 at Week 24 entered the study’s 24-week, double-blind, methotrexate withdrawal phase.
These patients were randomized to receive either extended-release tofacitinib with placebo methotrexate (tofacitinib monotherapy) or continue tofacitinib plus methotrexate (combination therapy). Change in Disease Activity Score-28 (DAS28)-4 for Rheumatoid Arthritis with ESR from Week 24 to 48 was the primary endpoint. Secondary endpoints included change in DAS28-4 (CRP), change in Simple Disease Activity Index (SDAI), change in CDAI, change in the Health Assessment Questionnaire Disability Index (HAQ-DI) and rates of ACR 20, 50 and 70 response. Non-inferiority of the treatments and safety were also assessed.
The Results
Of the 694 study patients, 530 patients achieved a CDAI score less than 10 at Week 24. Of these, 264 were randomized to receive tofacitinib monotherapy and 266 were randomized to receive tofacitinib plus methotrexate combination therapy. Demographics and patient characteristics were similar between the two treatment groups.
Patients on tofacitinib monotherapy demonstrated non-inferiority to tofacitinib plus methotrexate. Additionally, change in DAS28-4 (CRP), change in SDAI and change in CDAI were greater for the tofacitinib monotherapy group, but not clinically significant. The ACR/HAQ-DI responses on low disease activity rates were similar between the treatment groups. Additionally, rates of remission were similar between both groups, with no change after methotrexate withdrawal. In the double-blind phase, adverse events, serious adverse events and rates of drug discontinuation were comparable between the treatment groups.
This study demonstrated that patients who received extended-release tofacitinib plus methotrexate and achieved low disease activity can withdraw from methotrexate for up to 48 weeks without significant worsening of disease. Additionally, patients in remission usually stayed in remission after methotrexate withdrawal.
No new safety signals were identified. The safety profile appeared to be consistent with the known adverse event profile of tofacitinib.
Michele B. Kaufman, PharmD, BCGP, is a freelance medical writer based in New York City and a pharmacist at New York Presbyterian Lower Manhattan Hospital.