Brown VE, Pilkington CA, Feldman BM, Davidson JE. An international consensus survey of the diagnostic criteria for juvenile dermatomyositis (JDM). Rheumatology. 2006 Aug;45(8):990-993. Abstract and table reprinted with permission from the British Society for Rheumatology.
Abstract
Objective: To develop revised criteria for the diagnosis of juvenile dermatomyositis (JDM) using an international consensus process.
Methods: An initial survey was circulated to members of the Network for JDM and the Pediatric Rheumatology International Trials Organization (PRINTO). Each individual was asked to identify those criteria that were felt to be most helpful in the diagnosis of classical JDM. A second survey was derived from these results and used to rank these proposed criteria in order of their importance and usefulness in clinical practice.
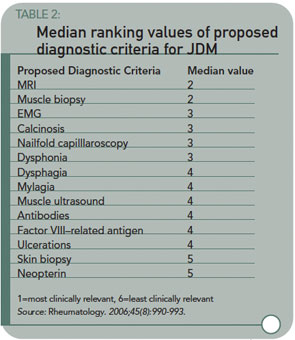
Results: The first survey had a response rate of 49.8% (118 individuals) from 92 centers in 32 countries. All responders routinely used proximal muscle weakness and characteristic skin rash in the diagnosis of JDM, while 86.8% used elevated muscle enzymes. Muscle biopsy, magnetic resonance imaging (MRI), and changes on the electromyogram (EMG) were deemed important diagnostic criteria. Other criteria, including myositis-specific or -related antibodies, nailfold capillaroscopy, factor VIII-related antigen, muscle ultrasound, calcinosis, and neopterin were used by 35.3% of respondents. Seventy-eight respondents to the first survey (66%) responded to the second survey. Typical MRI and muscle biopsy changes were rated by all to be the most useful clinically relevant diagnostic criteria after proximal muscle weakness, characteristic skin rash, and elevated muscle enzymes. These were followed by myopathic changes on EMG, calcinosis, dysphonia, and nailfold capillaroscopy, which were ranked equally.
Conclusion: This process identified nine criteria that clinicians felt to be helpful or important in the diagnosis of JDM. A further process of refinement and validation is necessary to agree on an internationally acceptable, clinically usable set of diagnostic criteria.
Commentary
Evidence-based medicine requires studies; studies require accepted, well-standardized criteria. The Bohan and Peters criteria for dermatomyositis have served internist-rheumatologists well for more than 30 years. Pediatric rheumatologists have also used these criteria to advantage to make JDM diagnosis. However with advances in imaging technologies and the reluctance of pediatricians (and parents) to subject children to invasive procedures, many clinicians have drifted from the strict use of these criteria, primarily avoiding muscle biopsies and EMGs while retaining rash, proximal weakness, and elevated enzymes.
The authors have started the process of updating criteria for JDMS by a survey/consensus technique, identifying the diagnostic methods currently used, and found useful, by pediatric rheumatologists. Table 2 lists the diagnostic methods and the median usefulness rank for each. (See Table 2, above.) Magnetic resonance imaging of edema/inflammation in proximal muscles is taking the vote as a potential substitute for biopsy or EMGs. This also has its problems—cost, availability, and the fact that young children need to be sedated to get decent images.