Back Pain
Stanton TR, Henschke N, Maher CG, et al. After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine. 2008;26:2923-2928.
Abstract
Study Design: Inception cohort study.
Objective: To provide the first reliable estimate of the one-year incidence of recurrence in subjects recently recovered from acute nonspecific low back pain (LBP) and to determine factors predictive of recurrence in one year.
Summary of background data: Previous studies provide potentially flawed estimates of recurrence of LBP because they do not restrict the cohort to those who have recovered and are therefore eligible for a recurrence.
Methods: We identified 1,334 consecutive patients who presented to primary care with acute LBP; of these 353 recovered before six weeks and entered the current study. The primary outcome measure was recurrence of LBP in the next year. Specifically, an episode of recurrence was defined in two ways: recall of recurrence at the 12-month follow-up and report of pain at the three- or 12-month follow-up. Risk factors for recurrence were assessed at the baseline. Pain intensity was assessed at six weeks, three months, and 12 months and recurrence at 12 months. Factors that could plausibly affect recurrence were chosen a priori and evaluated using a multivariable regression analysis.
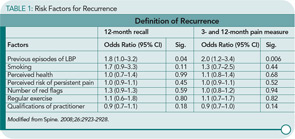
Results: Recurrence of LBP was found to be much less common than previous estimates suggest, ranging from 24% (95% CI=20–28%) using “12-month recall” definition of recurrence, to 33% (95% CI=28–38%) using “pain at follow-up” definition of recurrence. However, only one factor, previous episode(s) of LBP, was consistently predictive of recurrence within the next 12 months (odds ratio=1.8–2.0, P=0.00–0.05)
Conclusion: This study challenges the assumption that the majority of subjects with low back pain whose symptoms resolve will have a recurrence in a one-year period. After the resolution of an episode of acute LBP, about 25% of subjects will have a recurrence in the next year. Prediction of who will have a recurrence within the next year is difficult to determine.
Commentary
An acute episode of back pain is one of the most common afflictions of mankind. Studies have reported wide variations in the numbers of individuals who have experienced this malady. Seemingly, at one time or another, more people than are the world’s population have experienced pain in the area below the 12th rib and the crease of the buttocks. Although having one attack is bad enough, patients with back pain are at risk of a recurrence. Reports of the frequency of recurrences have ranged from 47% to 84% depending on the study population. An explanation for the wide range in the frequency of recurrences may be related to the definitions of recurrence. These definitions have been variously based upon pain, use of healthcare, or absence from work. For example, van den Hoogan et al reported a 75% recurrence rate based upon pain in 443 LBP subjects who responded to a postal questionnaire at 12 months.1 While relapses were less severe and of shorter duration than the initial episodes, no specific factors that predicted recurrence were identified in this study.