Abstract
Context: The 329,000 hip fractures that annually occur in the United States are associated with high morbidity, mortality, and cost. Identification of those at high risk is a step toward prevention.
Objective: To develop an algorithm to predict the five-year risk of hip fracture in postmenopausal women.
Design, setting, and participants: A total of 93,676 women who participated in the observational component of the Women’s Health Initiative (WHI), a multiethnic longitudinal study, were used to develop a predictive algorithm based on commonly available clinical features. Selected factors that predicted hip fracture were then validated by 68,132 women who participated in the clinical trial. The model was tested in a subset of 10,750 women who had undergone dual-energy X-ray absorptiometry (DXA) scans for bone mass density assessment.
Main outcome measure: The prediction of centrally adjudicated hip fracture, measured by the area under the receiver operator characteristic (ROC) curves.
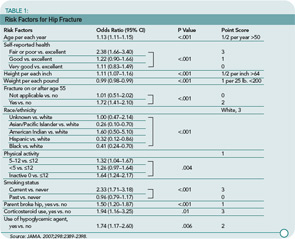
Results: During a mean (SD) follow-up of 7.6 (1.7) years, 1,132 hip fractures were identified among women participating in the observational study (annualized rate, 0.16%), whereas during a mean follow-up of 8.0 (1.7) years, 791 hip fractures occurred among women participating in the clinical trial (annualized rate, 0.14%). Eleven factors predicted hip fracture within five years: age, self-reported health, weight, height, race/ethnicity, self-reported physical activity, history of fracture after age 54 years, parental hip fracture, current smoking, current corticosteroid use, and treated diabetes. ROC curves showed that the algorithm had an area under the curve of 80% (95% confidence interval [CI], 0.77%–0.82%) when tested in the cohort of different women who were in the clinical trial. A simplified point score was developed for the probability of hip fracture. ROC curves comparing DXA-scan prediction based on a 10% subset of the cohort and the algorithm among those who participated the clinical trial were similar, with an area under the curve of 79% (95% CI, 73%–85%) versus 71% (95% CI, 66%–76%).
Conclusion: This algorithm, based on 11 clinical factors, may be useful to predict the five-year risk of hip fracture among postmenopausal women of various ethnic backgrounds. Further studies are needed to assess the clinical implication of the algorithm in general and specifically to identify treatment benefits.
Commentary
Hip fractures cause substantial morbidity, mortality, and related costs. While many pharmacologic agents have been developed for treating osteoporosis, an unacceptably high proportion of patients do not receive treatment until after a fracture, and many receive no treatment even after sustaining a fracture. Timely bone mineral density (BMD) testing can help identify at-risk individuals. However, most fractures occur in persons who do not have osteoporosis by t-score thresholds, pointing out the importance of non–BMD-related risk factors. Robbins and colleagues used the very large WHI datasets to develop and test a clinical prediction rule for hip fractures in postmenopausal women.