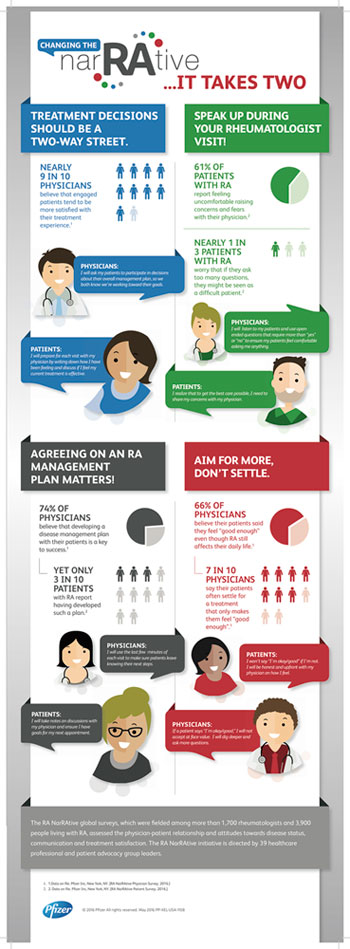
Two out of three patients living with rheumatoid arthritis (RA) say they feel “good enough,” even though their clinical assessments indicate active disease, according to the second phase of Pfizer’s global RA survey, the RA NarRAtive, which assessed the quality of physician–patient communication and its relationship to overall RA disease management.1
Two out of three patients living with rheumatoid arthritis (RA) say they feel “good enough,” even though their clinical assessments indicate active disease, according to the second phase of Pfizer’s global RA survey, the RA NarRAtive, which assessed the quality of physician–patient communication and its relationship to overall RA disease management.1
“The results illustrate that patients often experience communication difficulties with their physicians for a variety of reasons,” says RA NarRAtive Advisory Panel Co-Chair Allan Gibofsky, MD, a rheumatologist and co-director of the Inflammatory Arthritis Clinic at the Hospital for Special Surgery in New York. “This [difficulty] could be due to multiple factors, including a patient’s embarrassment in raising issues, a lack of time or a disconnect between a physician’s and patient’s assessment of the patient’s well-being. These potential communication gaps confirm the need for a joint commitment to improving dialogue focused on changing the narrative around RA management.”
The RA NarRAtive physician survey was conducted online in 15 countries by Harris Poll between August and October 2015, and respondents were 1,736 rheumatologists who had seen at least five patients in the previous month with moderate to severe RA.
“As a global initiative, it was somewhat surprising to learn that communication problems are universal and not necessarily unique to the U.S.,” says Dr. Gibofsky, who believes that it was important to get input from other countries because the practice of medicine is becoming more international in scope and focus.
More Takeaways
The survey’s findings also showed that the majority of physicians believe that setting treatment goals (78%) and developing a disease management plan (74%) with their patients is essential in successfully managing RA. According to most physicians, people living with RA who are involved in making treatment decisions tend to be more satisfied with their treatment experience than those who are not as involved.
But results from the first phase of the patient survey, which included input from 3,900 people living with RA, revealed that few patients have shared their treatment goals with their physician or even realize they have a disease management plan in place.
“Physicians are likely discussing both goals and disease management plans with their patients; however, patients may not [understand the plans] due to differences in the language or terminology physicians use when discussing these measures,” Dr. Gibofsky says.
Further, physician findings provided insight into similarities and differences in physician and patient perspectives. More than half of patients reported feeling uncomfortable raising concerns and fears with their physician, and many worried that if they asked too many questions, it would negatively affect their quality of care.
When reflecting on why some patients feel this way, Dr. Gibofsky believes that older patients tend to still view physicians as authority figures whom they shouldn’t contradict or interrupt, while younger patients are more assertive and challenging—perhaps because they have the ability to research a condition on the Internet. Cultural norms play a role as well.
Promoting Advocacy Groups
Although the survey reported that four of five physicians believe that patients who participate in RA support groups tend to be able to live better with RA, less than one-quarter of patients currently participate in a support or patient advocacy group.
“I think this is due to a lack of awareness or access to support groups and other services,” says Cindy McDaniel, a U.S. member of the RA NarRAtive Advisory Panel and senior vice president of Consumer Health & Impact for the Arthritis Foundation. The organization, the largest arthritis patient advocacy group in the world, has more than 20 support groups in communities throughout the country, plus online links to other community-based groups. In addition, the foundation offers free educational resources and tools for physicians and patients.
Ms. McDaniel says, “We encourage physicians to tell patients about us and what we can offer.” A new tool, called the Arthritis Research Finder, lets patients type in their ZIP code to see what types of resources are available within a certain radius of their home.
Improving Communication
So what can rheumatologists do to improve communication with patients? Dr. Gibofsky recommends physicians do the following:
- Whenever possible, allocate more time during appointments for discussions regarding the effect of disease on the patient’s quality of life. If necessary, schedule additional appointments.
- Understand that as a physician, you don’t have to address all of a patient’s concerns. Often, others—such as a nurse educator or practice management support group director—can address concerns that patients may not feel comfortable bringing up with the physician.
- Be sure your exam room is arranged so that it’s conducive to conversations. For example, make sure a computer screen is not positioned between the physician and patient, because this minimizes eye contact.
- Learn how to speak in the patient’s language. Realize they may not understand scientific terms or phrases. Pause every few sentences, and ask the patient if they understand what you’re saying.
- Encourage patients to ask open-ended questions; probe when necessary.
- Learn the skill of active, involved listening.
In addition, Ms. McDaniel suggests that physicians ask their patients to do the following:
- Encourage patients to do their homework, such as researching their condition and treatment options on the Internet, before an appointment.
- Encourage patients to be honest about how they feel now and on the days since their last appointment. Patients should discuss the biggest challenges and the things they miss out on due to having RA.
- Let patients know they can bring a relative or friend to their appointment. This person can provide a third-party perspective on how the patient is really feeling, especially if that patient may minimize their symptoms. The other person can also serve as another set of ears to understand and help reinforce what was said during the appointment afterward.
- Encourage patients to track their disease activity and the tasks they can and cannot do between visits to provide a good foundation for discussion during appointments.
What’s Next?
Now that the second phase of the survey is complete, the RA NarRAtive Advisory Panel, which is directed by 39 healthcare professional and patient advocacy group leaders, will work to develop tools and resources to help improve patient-physician dialogue identified by the study’s findings. These solutions will strive to change the narrative around RA to bridge gaps between beliefs and practices, and overall improve RA management.
“We always have better outcomes when patients are active partners in their care, particularly in the formulation of their management plan,” Dr. Gibofsky says. “I think the survey revealed some practical takeaways and highlighted things we can do better over time.”
Dr. Gibofsky concludes, “The bottom line is that people with RA should aim for more and not settle when it comes to treatment, because we can do so much more for them today than ever before. Each year brings a better understanding of RA, and new advances, therapies and practices. Patients can work aggressively with their physician to define and reach optimum status, taking advantage of all of the scientific breakthroughs that are revolutionizing care.”
Karen Appold is a medical writer in Pennsylvania.
Reference
- Pfizer Inc. News release: Global survey finds disconnects between physicians and people living with rheumatoid arthritis (RA). 2016 May 17.