Background/Purpose: Pegloticase, a recombinant, pegylated uricase, is used for treatment of gout in patients who fail oral urate lowering therapy (ULT). Despite successful reduction of urate levels and flares, its use is limited due to immunogenicity, leading to infusion reactions.1 Co-administration of an immunomodulatory agent may mitigate this loss of efficacy and concern for drug-related toxicity.
Methods: Patients from 5 rheumatology practices were recruited over 18 months, and randomized (3:1) by site to either to mycophenolate mofetil (MMF) 1 gram twice a day or placebo (PBO) with a run-in of two weeks prior to intravenous pegloticase at 8 mg every 2 weeks (12 infusions). MMF or PBO was given for the first 12 weeks. Inclusion criteria were: a) patients ≥18 years of age who met 2015 ACR/EULAR gout classification criteria and b) chronic refractory gout defined as symptoms inadequately controlled with ULT or contraindication to ULT. Endpoints included: a) proportion of subjects achieving and maintaining a serum urate (sUA) of ≤6 mg/dL at 12 weeks (primary), b) assess six-month durability of immune modulation after discontinuation of MMF at 12 weeks (secondary), and c) adverse events (AEs). Analyses were conducted using SAS (Cary, NC) Version 9.4 with Fisher’s exact test for binary outcomes and Wilcoxon two-sample test for continuous outcomes. Kaplan-Meier estimates and log-rank test were performed to compare survival curves between groups. Hypothesis tests were two tailed, and a P value (P) of <0.05 indicated statistical significance.
Results: Of 42 subjects screened, 35 were randomized, and 32 who received at least one dose of pegloticase were included in modified intention to treat analyses (Table 1: demographics). Nineteen of 22 (86%) in the MMF arm achieved the primary outcome at 12 weeks of sUA ≤6mg/dL, compared with four of 10 (40%) in placebo, P value 0.01. At week 24, sUA response was sustained in 68% of MMF arm vs. 30% in placebo. Estimated rates of AEs per month were similar between groups—MMF (0.3) and placebo (0.4). The MMF arm had higher AEs compared with placebo: musculoskeletal (36% vs. 10%), respiratory (18% vs. 0%) and infections (9% vs. 0%). The placebo arm had a greater percentage of infusion reactions (30% vs. 0%). Figure 1 demonstrates that the percentage of subjects maintaining a sUA <6 mg/dL at 12 weeks was significantly higher (P=0.02) in the MMF arm, and a significant difference (P=0.03) at 24 weeks indicating sustained benefit from MMF.
Conclusion: Short-term concomitant use of MMF with pegloticase was generally well tolerated in our proof-of-concept study. It was associated with a statistically significant and clinically meaningful impact on the proportion of subjects achieving and maintaining a sUA ≤6 mg/dL at 24 weeks. To our knowledge, this is the first randomized controlled trial to demonstrate prolonged efficacy of pegloticase with co-administrations of an immunomodulatory agent.
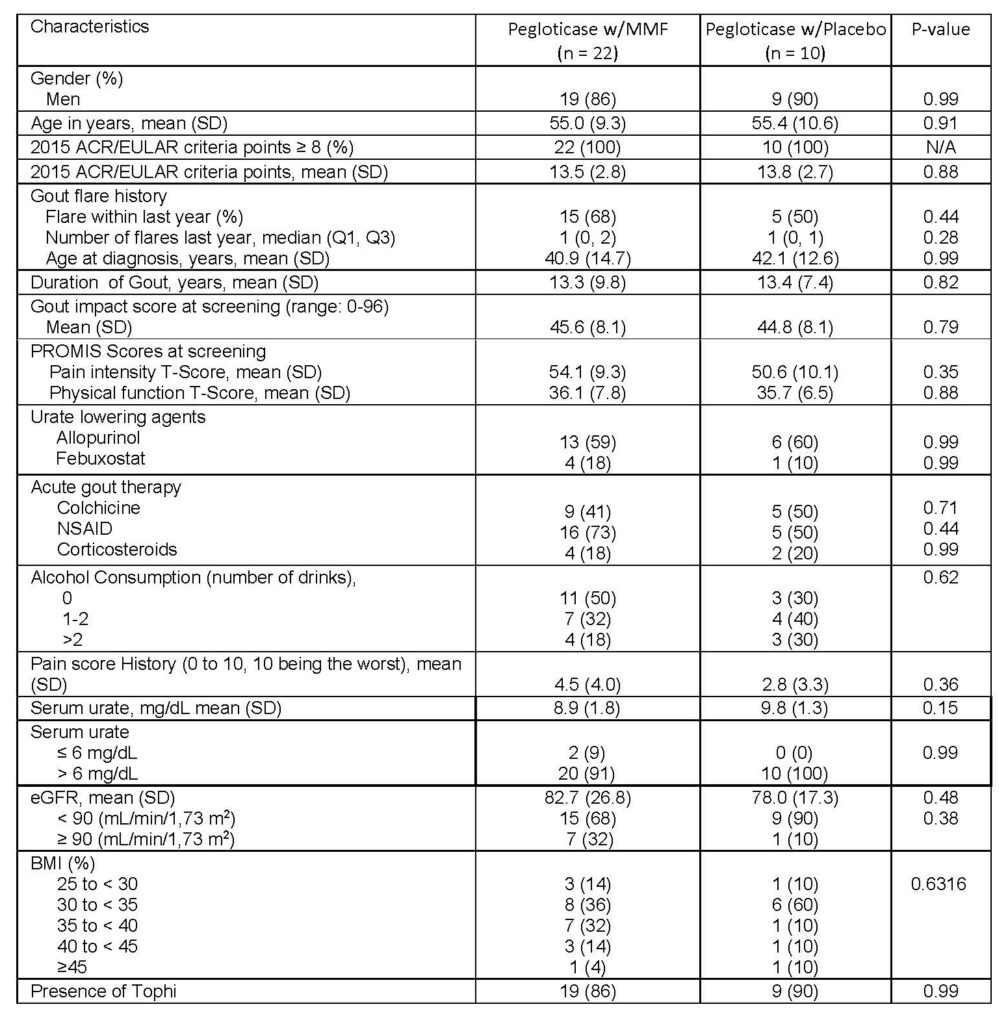
Table 1. Patient demographics for treatment arms of pegloticase with MMF and pegloticase with placebo
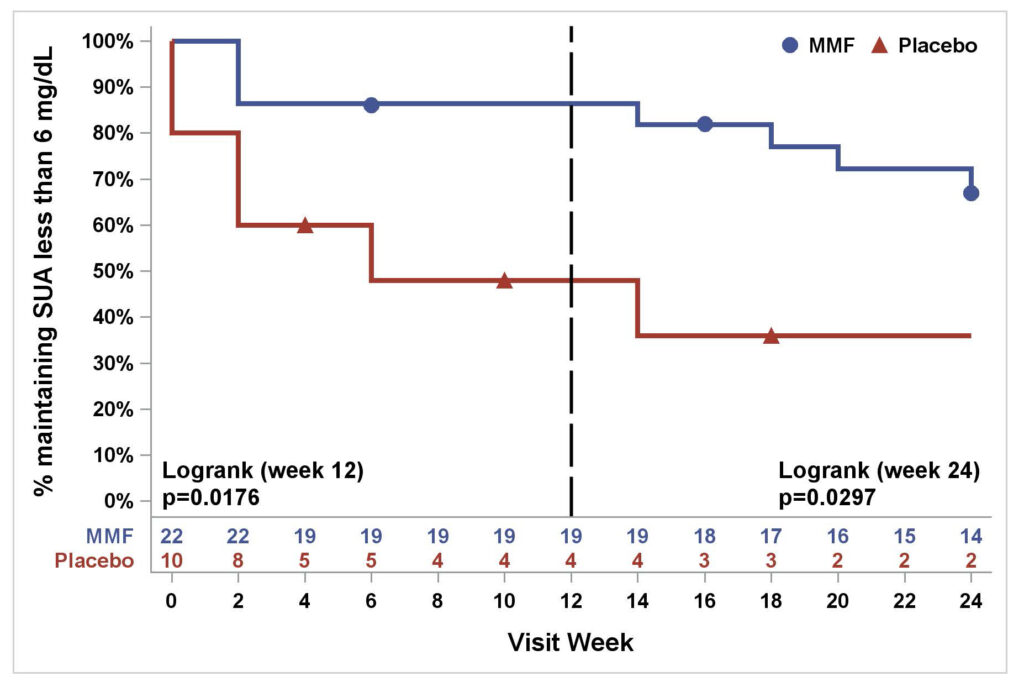
Figure 1. Percentage of subjects maintaining SUA less than 6 mg/dL in MMF/pegloticase vs. PBO/pegloticase arms over 24 weeks (Kaplan‐Meier estimates)
Puja Khanna1, Dinesh Khanna1, Gary Cutter2, Jeffrey Foster2, Joshua Melnick3, Sara Jaafar1, Stephanie Biggers2, AKM Rahman2, Hui-Chen Kuo2, Michelle Feese2 and Kenneth Saag4: 1University of Michigan, Ann Arbor; 2University of Alabama at Birmingham; 3University of Alabama at Birmingham, Vestavia Hills; 4University of Alabama at Birmingham, Division of Clinical Immunology and Rheumatology.
Disclosures: P. Khanna, Selecta, 5, Dyve, 5; D. Khanna, Bayer, 2, BMS, 2, Horizon, 2, Pfizer, 2, NIH, 2, Immune Tolerance Network, 2, Eicos Sciences Inc, 4, Acceleron,, 5, Actelion,, 5, Abbvie,, 5, Amgen,, 5, Bayer,, 5, Boehringer Ingelheim, 5, CSL Behring, 5, Corbus,, 5, Galapagos,, 5, Genentech/Roche, 5, GSK, 5, Horizon, 5, Merck,, 5, Mitsubishi Tanabe Pharma, 5, Sanofi-Aventis, 5, United Therapeutics, 5, Impact PH, 9, Scleroderma Development, 6, CiviBioPharma/Eicos Sciences Inc, 6; G. Cutter, Horizon Pharmaceuticals, 9, Biogen, 5, Click Therapeutics, 5, Genentech, 5, Gilgamesh Pharmaceuticals, 5, GW Pharmaceuticals, 5, Genzyme, 5, Klein-Buendel Incorporated, 5, Medimmune, 5, Medday, 5, Novartis, 5, Osmotica Pharmaceuticals, 5, Perception Neurosciences, 5, Perception Neurosciences, 5, Recursion Pharmaceuticals, 5, Roche, 5, Somahlution, 5, TG Therapeutics, 5; J. Foster, None; J. Melnick, None; S. Jaafar, None; S. Biggers, None; A. Rahman, None; H. Kuo, None; M. Feese, None; K. Saag, Arthrosi, 5, Horizon Therapeutics plc, 2, 5, Atom Bioscience, 5, LG Pharma, 5, Takeda, 5, Mallinkrodt, 5, SOBI, 2, 5, Shanton, 2.
Abstract number 0952, presented at ACR Convergence 2020.
To cite this abstract in AMA style:
Khanna P, Khanna D, Cutter G, Foster J, Melnick J, Jaafar S, Biggers S, Rahman A, Kuo H, Feese M, Saag K. Reducing Immunogenicity of Pegloticase (RECIPE) with Concomitant Use of Mycophenolate Mofetil in Patients with Refractory Gout—a Phase II Double Blind Randomized Controlled Trial [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/reducing-immunogenicity-of-pegloticase-recipe-with-concomitant-use-of-mycophenolate-mofetil-in-patients-with-refractory-gout-a-phase-ii-double-blind-randomized-controlled-trial.
 Click here to view abstract video
Click here to view abstract video Click here to view visual abstract summary
Click here to view visual abstract summary