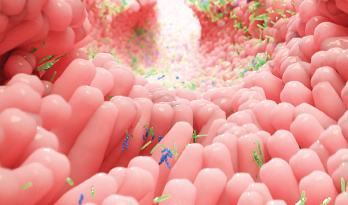
Alpha Tauri 3D Graphics / shutterstock.com
A growing body of research is elucidating the role of intestinal microbiota in several autoimmune diseases, including rheumatoid arthritis (RA). Research published in December 2018 Arthritis & Rheumatology increases our understanding of the “extent and nature of mucosal immune activation during preclinical arthritis.”1
The research objective, according to the report, was to “dissect intestinal mucosal immune responses in the preclinical phase of arthritis and determine whether the presence of Th17 cells, beyond involvement of the cytokine interleukin-17 (IL-17), is required for arthritis development and whether the involvement of Th17 cells in arthritis depends on the composition of the host microbiota.”
The research, using murine models of inflammatory arthritis, suggests that activation of mucosal immunity precedes the development of arthritis and that Th17 cells have a microbiota-dependent role in arthritis. These models (collagen-induced arthritis and antigen-induced arthritis) involve injections into the skin and/or joints, without direct exposure of the gut to antigen.
One of the researchers, Marije I. Koenders, PhD, assistant professor of experimental rheumatology at Radboud University Medical Center, Nijmegen, The Netherlands, explains the findings “demonstrate initiation of mucosal Th1 and Th17 cell responses and marked production of tumor necrosis factor α [TNFα], granulocyte-macrophage colony-stimulating factor [GM-CSF], and IL-22 by mucosal CD4+ T cells just before the clinical onset of arthritis.
“This suggests that activation of intestinal mucosal T cells during the immune-priming phase of RA may contribute to early, preclinical processes,” she says.
Although no direct application exists for this murine model-based research in clinical practice at this time, Dr. Koenders says microbiome-guided stratification of patients with inflammatory arthritis may improve therapeutic efficacy in the future.
“A microbiota that drives a string Th17 profile in arthritis patients may be a good indication for, for example, anti-IL-17 treatment or RORɣT blocking, whereas other microbiota may suggest a less important role for the Th17 pathway in disease,” she says.
“Currently, we are expanding our research in a model closer to the clinical situation. We are creating a humanized mouse model with human (patient-derived) microbiota in our mice to study the role of the microbiome in a highly translational setting to gain more insight into the mucosal cytokine responses and immunological consequences during arthritis development, especially in patients with new-onset RA.”
Role of the Microbiome
Research has found the composition of intestinal microbiota is altered in patients with RA. Patients with recent onset RA in North America have been found to have an increased amount of Prevotella copri and a reduced amount of Bacteroides in the gut.2
Subgroups of patients with RA have differential immunoglobulin G (IgG) or IgA immune reactivity with P. copri. A recent study found that about half of patients with RA have T cell responses to P. copri, responses that were either IgA antibody responses to P. copri, suggesting a mucosal immune response, or IgG antibodies to the organism, suggesting a systemic immune response.3
Mucosal surfaces—periodontal, lung, and intestinal tissues—are the proposed site of immune activation and breach of tolerance in RA, according to recent research, but the extent and nature of the mucosal immune activation during preclinical arthritis have been unclear.4
Researchers speculate that microbiome-guided stratification of patients with inflammatory arthritis may improve therapeutic efficacy in the future.
Several studies have demonstrated perturbed diversity and composition of commensal microbiota in patients with RA compared with healthy individuals.5-8 However, the relationship between dysbiosis and the pathogenesis of RA is not fully understood, said Dr. Koenders and colleagues in their article.
Dysbiosis, or microbial abnormalities, may be related to several types of diseases. Intestinal dysbiosis has been observed in inflammatory bowel disease and in diseases that affect the tissues of the gut, according to an article in the Journal of Clinical Medicine.2 Dysbiosis of the microbiota has been identified in patients with type 1 diabetes, multiple sclerosis, autism, and in patients with RA in the U.S., China, and Finland, the researchers say.2

Dr. Koenders
Dr. Koenders notes many studies have proposed a role for microbiota-induced Th17 cells in arthritis development. Even though previous animal studies have shown that Th17 cell-inducing intestinal microbiota exacerbate experimental arthritis in mice, it was not yet known whether involvement of these microbiota-induced Th17 cells was actually required for the pathogenesis of the disease, she says.
“Our studies using Th17 cell-deficient mice showed that Th17 cells are required for the progression of arthritis and affect several features of structural joint pathology in two murine arthritis models.
“Interestingly, with the known role of other cellular sources of IL-17 in arthritis in mind, we demonstrated, using an elegant transgenic mouse model, the specific, differential contribution of Th17 cells as a main source of IL-17, as well as an important producer of other proinflammatory mediators like GM-CSF and IL-22,” Dr. Koenders says.
A novel finding of the study is that the production of GM-CSF and IL-22 by small intestine lamina propria Th17 cells is increased during preclinical arthritis. These cytokines, she says, are implicated in the pathogenesis of RA and may have IL-17-independent proinflammatory and osteoclastogenic functions.
“Our research emphasizes that the role of Th17 cells goes beyond IL-17-dependent arthritis processes and also drives IL-22 and GM-CSF-mediated arthritis,” says Dr. Koenders.
Kathy Holliman, MEd, has been a medical writer and editor since 1997.
References
- Evans-Marin H, Rogier R, Koralov SB, et al. Microbiota-dependent involvement of Th17 cells in murine models of inflammatory arthritis. Arthritis Rheumatol. 2018 Dec;70(12):1971–1983.
- Maeda Y, Takeda K. Role of gut microbiota in rheumatoid arthritis. J Clin Med. 2017 Jun 9;6(6):pii: E60.
- Pianta A, Arvikar S, Strle K, et al. Evidence of the immune relevance of Prevotella copri, a gut microbe, in patients with rheumatoid arthritis. Arthritis Rheumatol. 2017 May;69(5):964–975.
- Rosenbaum JT, Asquith MJ. The microbiome: A revolution in treatment for rheumatic diseases? Curr Rheumatol Rep. 2016 Oct;18(10):62.
- Scher JU, Sczesnak A, Longman RS, et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. Elife. 2013 Nov 5;2:e01202.
- Maeda Y, Kurakawa T, Umemota E, et al. Dysbiosis contributes to arthritis development via activation of autoreactive T cells in the intestine. Arthritis Rheumatol. 2016 Nov;68(11):2646–2661.
- Zhang X, Zhang D, Jia H, et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med. 2015 Aug;21(8):895–905.
- Chen J, Wright K, Davis JM, et al. An expansion of rare lineage intestinal microbes characterizes rheumatoid arthritis. Genome Med. 2016 Apr 21;8(1):43.


