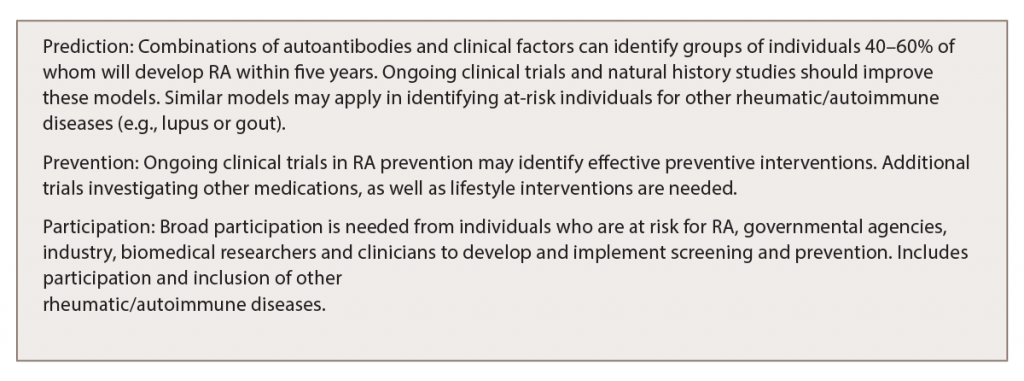
One of the primary issues to address is the development of methods to identify individuals who are at high risk for future RA in a large-scale, clear and cost-effective manner. This will depend to a large extent on the accuracy, availability and cost of screening approaches to identify at-risk individuals.
ACPA and RF testing, along with assessment of other factors, appears in prospective studies to identify groups in whom ~40–60% develop synovitis and classifiable RA within two to five years of follow-up. These are fairly high positive predictive values (PPVs) that are currently deemed strong enough to drive the development of clinical trials, but broad screening of the healthy population would be the next step for implementation. ACPA and RF testing are widely clinically available, so conceivably these tests could be utilized in broader screening and prevention programs.
These predictive models have been developed in relatively small populations when compared with the overall numbers of individuals worldwide with established RA, as well as the number of individuals who may be ACPA positive and not have synovitis. As such, prediction models will need to be refined as the numbers of subjects who are at risk for RA are studied as part of ongoing clinical trials and other natural history studies.
Importantly, development of screening approaches for individuals who may benefit from RA prevention also entails identifying which groups are most appropriate to evaluate. Certain populations are at increased risk for RA; therefore, these may be the groups to initially target for prevention. These groups include family members of individuals with established disease, as well as certain racial groups, such as North American natives.15,16
Predictive models for RA are being developed and refined in these clinical trials, as well as in ongoing natural history studies of the development of RA in the U.S., Canada, Europe and elsewhere.17,18 If it is shown that RA prevention works, and is cost effective and reasonably safe, general population-based approaches to identify individuals at risk for RA may be developed, such as broad ACPA testing (or testing for other biomarkers) performed routinely, much like cholesterol and hemoglobin A1c are tested (and treated) in primary care settings.
(click for larger image) Table 1: Challenges & Opportunities in Preventing RA & Other Rheumatic Diseases
Interventions
Another critical factor in prevention is to define the appropriate intervention that balances efficacy with tolerability, acceptability and cost. Several drugs are being tested in the current RA prevention trials (e.g., hydroxychloroquine, abatacept), each targeting different biologic pathways. If one of these drugs rises to the top in terms of efficacy, that may be the first agent to be used widely. However, multiple agents will likely need to be evaluated, and safety and cost would be important considerations. In addition, new pharmacologic agents could be developed to target specific pathways that may be more relevant in preclinical RA, because we cannot assume that drugs that work well in the clinically apparent phase of disease are necessarily ideal for prevention.
Alternatives to Drugs
Other factors to prevent RA are as important and effective as drugs, especially if implemented in individuals who do not yet have clinically apparent arthritis. Established and emerging evidence exists that smoking cessation may reduce RA risk, and some evidence indicates that a healthy diet, increased consumption of fish and certain other dietary factors, weight loss and exercise may reduce the risk of RA.19-22