One difference observed in isolated RPF is that the tissue does not have as many IgG4+ plasma cells, but also fewer cells in general. “This can result in lower overall IgG4+ plasma cells, but a higher IgG4/IgG ratio, where almost all plasma cells in a biopsy are IgG4 positive, for example,” Dr. Stone explained.
Also, a subset of non-IgG4-related RPF that is poorly understood to date is characterized on biopsy with acellular fibrosis and small lymphoid aggregates, and sometimes entrapped, necrotic fat cells.
Dr. Stone explained how RPF should be considered on a spectrum with IgG4-RD, with significant overlap in some patients. He provided the example of the polymyalgia rheumatica/giant cell arteritis spectrum as a similar parallel to the association of RPF and IgG4-RD.
Two subtypes of IgG4-RD are a fibrotic subtype and proliferative subtype. The fibrotic subtype has low frequency of atopy, typically normal serologic activity (normal IgG4, eosinophils and complement levels), and pathology with sparse IgG4+ cells per HPF but an IgG4/IgG ratio usually greater than 40%. The proliferative subtype of IgG4-RD has high prevalence of atopy, often serologic activity (elevated IgG4 levels, eosinophilia, hypocomplementemia), high numbers of IgG4+ plasma cells on biopsy in the lymphoplasmacytic infiltrate and very robust response to treatment.
Although RPF is classically grouped under the fibrotic subtype, Dr. Stone explained how some patients will have features similar to IgG4-RD and multisystem organ involvement.
Systemic Involvement Outside the Retroperitoneum
Dr. Stone noted that the traditional approach to RPF, which even he adopted for many years, as “typically confined to the retroperitoneum is really not true.”
In the cohort at Massachusetts General Hospital, Dr. Stone noted they have treated 571 IgG4-RD patients, of which 22% (124) have RPF. Among these cases of RPF, 56 have RPF only and 68 have RPF with other organ involvement. For example, 47% of patients with RPF in the MGH cohort (who fulfill ACR/EULAR classification criteria) have pancreatic disease, 43% have submandibular gland disease, 39% have renal involvement and 25% have aorta or large vessel disease (see Table 2).
“If you look down the list of organs involved [in RPF], it reads like any large cohort of patients with IgG4-related disease,” Dr. Stone said.
| Table 2: Organ Involvement in RPF |
|---|
| Pancreas (47%) |
| Submandibular Gland (43%) |
| Kidney (39%) |
| Aorta/Large Vessels (25%) |
| Lacrimal Gland (22%) |
| Lymph Node (22%) |
| Lungs (20%) |
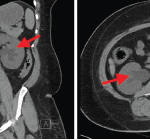
Caution of RPF Mimics, Especially Malignancy
For the latter part of the talk, Dr. Stone reviewed clinical cases that he has managed and offered some cautious pointers for clinicians in managing these patients.