WASHINGTON, D.C.—Retroperitoneal fibrosis (RPF) is often a challenging diagnosis to make, given a lack of serologic biomarkers and often difficulty in accessing tissue for biopsy, especially in cases confined to the retroperitoneum. The topic of retroperitoneal fibrosis was discussed during the CARE to Test Your Knowledge: Retroperitoneal Fibrosis session at ACR Convergence 2024.
John Stone, MD, MPH, professor of medicine at Harvard Medical School, Boston, the Edward A. Fox Chair in Medicine at Massachusetts General Hospital (MGH), Boston, and the executive chair of the IgG4ward! Foundation, provided an overview of an approach to RPF and important considerations in its diagnosis and management.
4 Management Principles
Dr. Stone noted four principles that rheumatologists should know about RPF. The first principle is that most cases of idiopathic RPF are probably IgG4-related disease (IgG4-RD), or at least should be treated that way. The second principle is that there is an important differential diagnosis that one must cautiously work through.
“The differential diagnosis includes, most importantly, malignancy, such as sarcoma, lymphoma or metastatic carcinoma, which can mimic retroperitoneal fibrosis,” Dr. Stone said. Primary amyloidosis, Erdheim-Chester disease, sarcoidosis or tuberculosis are also entities in the differential that may mimic RPF (see Table 1).
His third principle is that a lot remains to be known about RPF.
And finally, the fourth principle is to not fear RPF: “This disease … is responsive to therapy and patients do well,” Dr. Stone said.
| Table 1: RPF DDx: Mimics of Retroperitoneal Fibrosis |
|---|
| Malignancy • sarcoma • lymphoma • metastatic carcinoma |
| Primary Amyloidosis |
| Erdheim-Chester Disease |
| Sarcoidosis |
| Tuberculosis |
RPF on a Spectrum with IgG4-RD
Dr. Stone then made a case for why RPF should be considered as part of the spectrum of IgG4-RD, which he noted may seem surprising as RPF often feels different than IgG4-RD. Unlike IgG4-RD, patients with RPF have typically normal serum IgG4 levels, are serologically inactive (with absence of hypocomplementemia, normal IgE levels), often have single-organ involvement (confined to the retroperitoneum) and are slowly responsive to therapy.
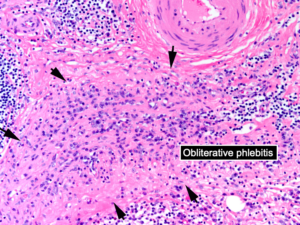
Despite these clinical differences, Dr. Stone argued that pathology is a clue linking these two entities, given similar histopathologic findings on biopsy. IgG4-RD is characterized by lymphoplasmacytic infiltrate on biopsy with many plasma cells staining for IgG4 and often a distinct pattern of storiform fibrosis and obliterative phlebitis of blood vessels, particularly veins (see Figure 1). “This is exactly what is seen in retroperitoneal fibrosis as well,” Dr. Stone said.
One difference observed in isolated RPF is that the tissue does not have as many IgG4+ plasma cells, but also fewer cells in general. “This can result in lower overall IgG4+ plasma cells, but a higher IgG4/IgG ratio, where almost all plasma cells in a biopsy are IgG4 positive, for example,” Dr. Stone explained.
Also, a subset of non-IgG4-related RPF that is poorly understood to date is characterized on biopsy with acellular fibrosis and small lymphoid aggregates, and sometimes entrapped, necrotic fat cells.
Dr. Stone explained how RPF should be considered on a spectrum with IgG4-RD, with significant overlap in some patients. He provided the example of the polymyalgia rheumatica/giant cell arteritis spectrum as a similar parallel to the association of RPF and IgG4-RD.
Two subtypes of IgG4-RD are a fibrotic subtype and proliferative subtype. The fibrotic subtype has low frequency of atopy, typically normal serologic activity (normal IgG4, eosinophils and complement levels), and pathology with sparse IgG4+ cells per HPF but an IgG4/IgG ratio usually greater than 40%. The proliferative subtype of IgG4-RD has high prevalence of atopy, often serologic activity (elevated IgG4 levels, eosinophilia, hypocomplementemia), high numbers of IgG4+ plasma cells on biopsy in the lymphoplasmacytic infiltrate and very robust response to treatment.
Although RPF is classically grouped under the fibrotic subtype, Dr. Stone explained how some patients will have features similar to IgG4-RD and multisystem organ involvement.
Systemic Involvement Outside the Retroperitoneum
Dr. Stone noted that the traditional approach to RPF, which even he adopted for many years, as “typically confined to the retroperitoneum is really not true.”
In the cohort at Massachusetts General Hospital, Dr. Stone noted they have treated 571 IgG4-RD patients, of which 22% (124) have RPF. Among these cases of RPF, 56 have RPF only and 68 have RPF with other organ involvement. For example, 47% of patients with RPF in the MGH cohort (who fulfill ACR/EULAR classification criteria) have pancreatic disease, 43% have submandibular gland disease, 39% have renal involvement and 25% have aorta or large vessel disease (see Table 2).
“If you look down the list of organs involved [in RPF], it reads like any large cohort of patients with IgG4-related disease,” Dr. Stone said.
| Table 2: Organ Involvement in RPF |
|---|
| Pancreas (47%) |
| Submandibular Gland (43%) |
| Kidney (39%) |
| Aorta/Large Vessels (25%) |
| Lacrimal Gland (22%) |
| Lymph Node (22%) |
| Lungs (20%) |
Caution of RPF Mimics, Especially Malignancy
For the latter part of the talk, Dr. Stone reviewed clinical cases that he has managed and offered some cautious pointers for clinicians in managing these patients.
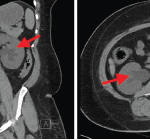
The classic distribution radiographically that favors IgG4-related RPF includes peri-aortic inflammation, typically infrarenal and extending to the iliac arteries, which sometimes entrap the ureters causing hydronephrosis.
“When [radiographic findings] are not in the classic distribution, I worry,” Dr. Stone said. “These are the cases where one can be burned.” He noted even when biopsied to rule out malignancy, the needle may go into a peri-tumoral location around a tumor where pathology can mimic IgG4-RD and miss cancer. “Only later when the patient is not responding as anticipated does it become clear it was a malignancy all along,” he said.
One tip in cases not fitting a classic radiographic distribution is to obtain biopsy to confirm histopathology and to follow patients for clinical and radiologic response. Some additional pointers of precaution are that fevers are highly atypical for IgG4-RD, so one needs to consider alternative diagnoses like malignancy (lymphoma) or Erdheim-Chester disease in patients with fever. Additionally, bulky lymphadenopathy (greater than 2 cm) is also very atypical and should be biopsied.
In Sum
This CARE session on RPF provided attendees a review of RPF including role of biopsy, important mimics in the differential not to miss, and considering RPF as an entity on the spectrum with IgG4-RD. By better characterizing RPF, hopefully this can improve diagnosis and development of future therapeutics. “I know there is a great deal of uncertainty about RPF, but I feel we are poised to make a lot of progress, finally, in this area over the next few years,” Dr. Stone said.
Mithu Maheswaranathan, MD, is an assistant professor of medicine in the Division of Rheumatology at Duke University School of Medicine in Durham, N.C.