The patient was discharged on 60 mg/day of prednisone with the recommendation to be slowly tapered as an outpatient. Table 1 (below) depicts the values of creatinine and proteinuria at admission, discharge and two-, six- and nine-month follow-up points. Over time, both renal function and level of proteinuria improved significantly.

TABLE 1: Creatinine (mg/dL), eGFR (mL/min/1.73 m2) and urine protein/creatinine ratio (mg/g) at admission, discharge,
2-, 6- and 9-month follow-up
Discussion
Renal dysfunction pathophysiology in RA patients is frequently linked to secondary amyloidosis due to long-lasting chronic inflammation.1,2 Rarely, the etiology of renal involvement is reported to be secondary to renal vasculitis or an autoimmune process. A review of literature resulted in sparse case reports of RA patients who developed minimal change disease, mesangial proliferative, focal segmental/proliferative or fibrillary glomerulonephritis (GN).6
Drug-induced glomerulopathies are most likely immune mediated, and they can present with a nephritic or nephrotic syndrome. Focal segmental glomerulosclerosis, mesangial crescentic and MPGN have been reported. Patients with HLA-B8 and DR3 antigens are more susceptible for drug-induced GN.7,8
In an effort to find if she is predisposed to develop a drug-induced autoimmune GN, our patient was HLA typed. She carried the following HLA class I antigens: A1, B8, B62, C3, C7 and class II antigens DR4, DR17, DQA1 03; 05, DQB1 02; 03. As previously mentioned, carriers of HLA-B8 antigens are predisposed to drug-induced GN, and HLA-DR4 antigens are known to be slow acetylators.9
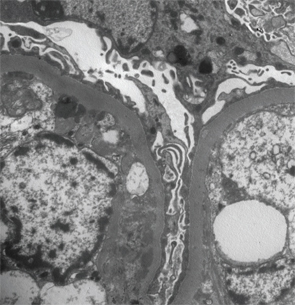
Figure 2: Renal biopsy. Electron microscopy: irregular thickening of the glomerular basement membrane with a few scattered subendothelial electron dense deposits, focal neomembrane formation, an expanded mesangium and podocyte foot processes effacement.
Exposure to TNF-alpha inhibitors, particularly in RA, is associated with membranous or necrotizing crescentic GN.6 Piga et al performed a review of the literature of patients with chronic inflammatory rheumatic diseases treated with biologics who developed autoimmune renal disorders.10 Interestingly, 22 out of 29 cases were RA patients, with Etanercept being the cause in about 51% of cases, followed by adalimumab (31.0%), infliximab (10.3%), tocilizumab and abatacept (3.4% each).10 Drug-induced lupus due to TNF-alpha inhibitors manifested clinically with rash (73%), polyarthritis (52%), fever (52%), myalgias (24%), pericardial effusion (9%) and, rarely, with nephritis (9%).3,4
Common features in TNF-alpha drug-induced GN were proteinuria, hypocomplementemia and positive SSA antibodies, although in the majority of cases, the renal dysfunction was reported during the time of the therapy with significant improvement after discontinuation.4,11

