For most rheumatologists and patients, the first two options are nonstarters. The third option is fraught with obstacles, including a shortage of rheumatologists in many locales.8 Most RAPP clinicians now agree that the fourth option, changing how we assess disease activity, is a breakthrough opportunity for improving our efficiency, costs and quality of care.
What is clear to us is that population management is the key to resolving the visit capacity bottleneck. Evidence for this has been generated by exemplar practices in other medical specialties that also manage chronic diseases in diverse practice environments.9 Population management enables clinicians to provide timely disease activity measurement and recommended care. It requires adopting better-defined systems of care that include:
- Disease registries to track required work, performance and disease outcomes;
- Clinical workflow standardization and care algorithms;
- Standardized disease activity measures; and
- A team approach within health systems and practices.
Of the 168 busy rheumatology practices participating in the RAPP Project, about 90 to date are implementing population-management capabilities, and the number continues to grow as clinicians are able to resolve practice- and system-level barriers.
To begin, we are each fully enrolling our RA population into a disease registry and subsequently identifying all of our patients who are overdue for disease activity assessments. Then to further address the bottleneck, many of us are reorganizing our practice care teams and assessments in innovative ways. Here are a few examples:
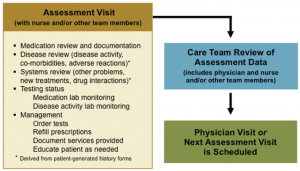
- Some practices are scheduling assessment visits with nurses and/or mid-level providers at least two weeks before physician visits to collect each physician’s preferred disease activity data and medication safety data (see Figure 4). These visits provide a more complete, consistent and well-organized dataset for the physician-patient encounter.
- Based on these disease activity data, rheumatologists, mid-level providers, and nurses are determining at the point of service who will see which patients. Physicians focus on more complex patients, other team members provide care for established patients with less complicated needs, and the practice’s total visit capacity increases significantly.
- In fact, once this division of effort is implemented, some physicians are hiring additional mid-level providers to right size their teams.
- Once a patient’s lab results are returned (see first bullet above), some care teams are reviewing their assessment visit data and deciding whether the patient requires a provider visit at all. Patients with well-controlled RA and no other problems are being rescheduled instead for a future assessment visit. This is freeing physician visit slots, enabling the physician to promptly see patients with high disease activity and other pressing management needs. (These reviews can be completed in batches rather than one patient at a time.)
- Embedding a pharmacist as an additional provider within the practice team is one highly intriguing option being implemented by some RAPP physicians. By managing medications, solving medication-related problems, and educating patients the pharmacist further reduces the physician’s workload.
As a result of these improvements, RAPP practices are beginning to report positive revenue impacts through an increase in visits and other services that address previously unmet patient needs. Moreover, some are adding technician-performed ultrasound and other clinical and educational services as individual patients require.
Removing the Physician Visit Bottleneck Enables Treat-to-Target Care
Many RAPP physicians, our practice teams, and most importantly our RA patients are enthusiastic about the benefits population management is providing for care and disease outcomes. We are now able to say with confidence, “My team manages this number of RA patients, their assessments are up to date, their treatments are necessary and safe, and their disease activity reflects the best we can possibly do for them.”