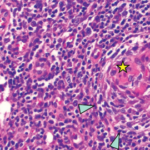
Figure 1
Due to lymphadenopathy and concern for lymphoma, an inguinal lymph node biopsy was performed by interventional radiology, but was non-diagnostic.
A bone marrow biopsy was performed and revealed normocellular bone marrow for the patient’s age.
Flow cytometry revealed no phenotypic evidence of blasts, myeloid dysmaturation, T cell lymphoma or plasma cell dyscrasia. Due to a domestic concern arising at this time, the patient signed out of the hospital against medical advice.
Two days later, she presented with night sweats and altered mental status (AMS). She had borderline low blood pressure of 91/60 mmHg and hypoxia with oxygen saturation of 70%. A CT angiogram was performed, which ruled out pulmonary embolism. The patient had an adequate response to fluid resuscitation. A CT scan of the head with and without contrast and lumbar puncture were negative; however, her AMS worsened and the patient was noted to laugh inappropriately and hear voices.
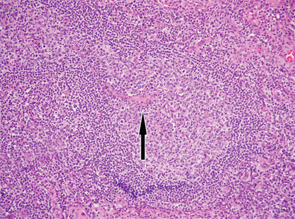
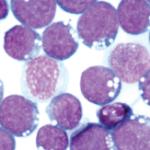
Figure 2
An excisional lymph node biopsy was performed and the autoimmune workup was repeated, because the clinical picture was consistent with SLE and scleroderma. The ANA came back positive with quantitative level of 638 IU/mL; anti-ds DNA, anti-SSB, anti-Sm, anti-RNP and anti-histone antibodies were also positive. Anti-Jo 1 was equivocal, and the anti-centromere, anti-SCL-70 and anti-RNA polymerase III were negative. Her serum protein electrophoresis revealed an elevated polyclonal spike suggestive of inflammatory process.
In light of the patient’s altered mental status, negative CNS workup, positive ANA, anti-ds DNA and anti-Sm, SLE with lupus cerebritis was diagnosed.
The patient was treated with pulse steroid therapy, followed by high-dose steroids, with moderate improvement in mental status and resolution of fever.
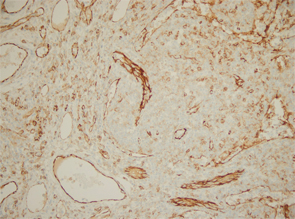
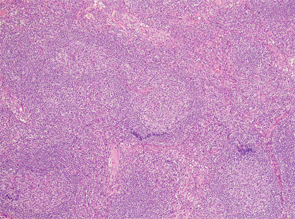
Excisional biopsy of a left inguinal lymph node. 1) Low magnification shows preserved architecture of the lymph node. 2) A germinal center with a central hyalinized vessel (arrow), giving a lollipop appearance. 3) Immunostaining using an endothelial cell marker, CD31, highlights the blood vessels.
Of note, the patient had digital ulceration and Raynaud’s phenomenon. An echocardiogram suggested pulmonary hypertension. The excisional lymph node biopsy revealed reactive lymphadenitis with features of MCD (see Figures 1–3, opposite). The lymph node specimen was negative for human herpes virus 8 (HH8). EBV IgM and IgG, as well as PCR, were positive.
The patient was treated with the IL-6 inhibitor, siltuximab. After the first dose of siltuximab, the patient had significant improvement of her mental status, and her overall performance returned back to her baseline. She continued to receive siltuximab as an outpatient, but did not follow up with the rheumatology clinic.