
gwolters / Shutterstock.com
Case
Ms. A is an 82-year-old woman who presented to the rheumatology office for evaluation of osteoporosis. She had been diagnosed with postmenopausal osteoporosis at age 62 after sustaining a right wrist fracture. She was started on alendronate 70 mg weekly and reported medication compliance. At age 79, she sustained an atraumatic right femur fracture. She was continued on alendronate at the same dosage by Physician 1. Three years later, she sustained a third fracture, an atraumatic left femur fracture.
An orthopedic surgeon repaired the left femoral fracture and referred her to a rheumatologist, Physician 2, for the management of her osteoporosis. The patient had no other medical problems. Physician 2 reviewed X-rays taken at the time of each of her femoral fractures. Each femoral fracture had a similar radiographic appearance, consistent with an atypical femoral fracture (AFF) (see Figure 1). Physician 2 discussed the diagnosis of AFFs with the patient and recommended discontinuation of alendronate, which she had taken for the past 20 years. Physician 2 recommended that she initiate a two-year course of teriparatide 20 mcg daily. The patient expressed concern about the decision of her former physician (Physician 1) to continue alendronate despite the fact that she had sustained a right femoral fracture at age 79. She was concerned that her medication continuation might have contributed to her developing a second AFF, on the contralateral side.
What should Physician 2 do next?
Discussion
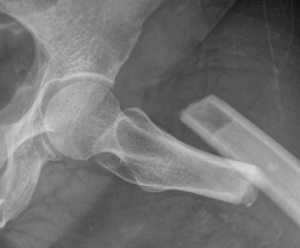
Figure 1: Subtrochanteric transverse fracture consistent with a left atypical femoral fracture.
Medical errors are defined as the failure of a planned action to be completed as intended or the use of a wrong plan to achieve an aim.1 Adverse events are injuries that result from a medical intervention and are responsible for harm to the patient.1 When medical errors lead to adverse events in patients, physicians should disclose them to their patients. A full disclosure of medical error involves communication between the healthcare provider and patient that includes admission of a mistake, discussion of the error and a conversation about the link from error to harm.2
Medical societies in the U.S. support full disclosure of medical errors that lead to adverse events.3,4 For example, the American Medical Association code of ethics states: “Situations occasionally occur in which a patient experiences significant medical complications that may have resulted from the physician’s mistake or judgment. Therefore, the physician is ethically required to inform the patient of all the facts necessary to ensure understanding of what has occurred.”4
