ARZTSAMUI/shutterstock.com
Ophthalmologists may be more likely to initially diagnose and treat scleritis, an inflammation of the scleral tissues of the eye. However, rheumatologists need to remain aware of the condition as well: It’s commonly associated with rheumatic disorders, such as rheumatoid arthritis (RA).
Scleritis can present in the eye anteriorly or posteriorly. “Anterior scleritis can be diffuse, nodular, necrotizing with inflammation and necrotizing without inflammation,” says ophthalmologist Gaston O. Lacayo, III, MD, Center for Excellence in Eyecare, Miami. “The most common clinical forms are diffuse scleritis and nodular scleritis.”
Although necrotizing scleritis is less common, it’s more ominous and frequently associated with systemic autoimmune disorders, Dr. Lacayo says.
There is also posterior scleritis, which is characterized by the flattening of the choroid and sclera and retrobulbar edema, Dr. Lacayo says. Posterior scleritis can negatively affect the vision, and it can be difficult to diagnose because it is not always seen during a slitlamp examination, says Esen K. Akpek, MD, The Bendann Family Professor of Ophthalmology and Rheumatology, and associate director, Johns Hopkins Jerome L. Greene Sjögren’s Syndrome Center, The Wilmer Eye Institute at Johns Hopkins, Baltimore.
Scleritis Symptoms
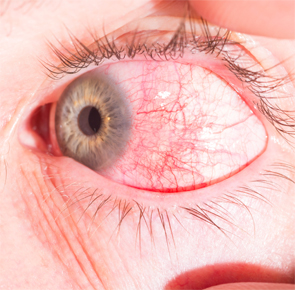
The symptoms of scleritis coincide with a number of eye problems. “It’s mostly redness and eye pain,” Dr. Akpek says. “The patients might get blurred vision if the posterior sclera is involved. Sometimes the inflammation spills over to the anterior chamber, causing uveitis. That also can cause blurred vision,” Dr. Akpek says.
If not treated properly, scleritis leads to blindness in severe cases.
Eye pain is sometimes so bad at night, it can cause trouble sleeping, says rheumatologist Elyse Rubenstein, MD, Providence Saint John’s Health Center, Santa Monica, Calif. Headaches and photophobia are other possible symptoms of scleritis.
These same symptoms can accompany conjunctivitis, iritis, keratitis, uveitis, herpes zoster and corneal melt, among other ocular disorders, Dr. Rubenstein says.
Treating physicians must also make the distinction between scleritis and the more benign episcleritis. “The redness in episcleritis is a brighter red, and in scleritis, it’s more bluish red,” Dr. Akpek says. “Also, with the exam, there’s scleral edema and deep episcleral vascular engorgement with scleritis.”
Slitlamp examination detects the intraocular inflammation in scleritis and assesses severity. CT scan, MRI and ultrasound are sometimes necessary to help determine the extent of involvement and make a differential diagnosis, says rheumatologist Anca Askanase, MD, clinical director and founder of the new Lupus Center at Columbia University Medical Center, New York.

