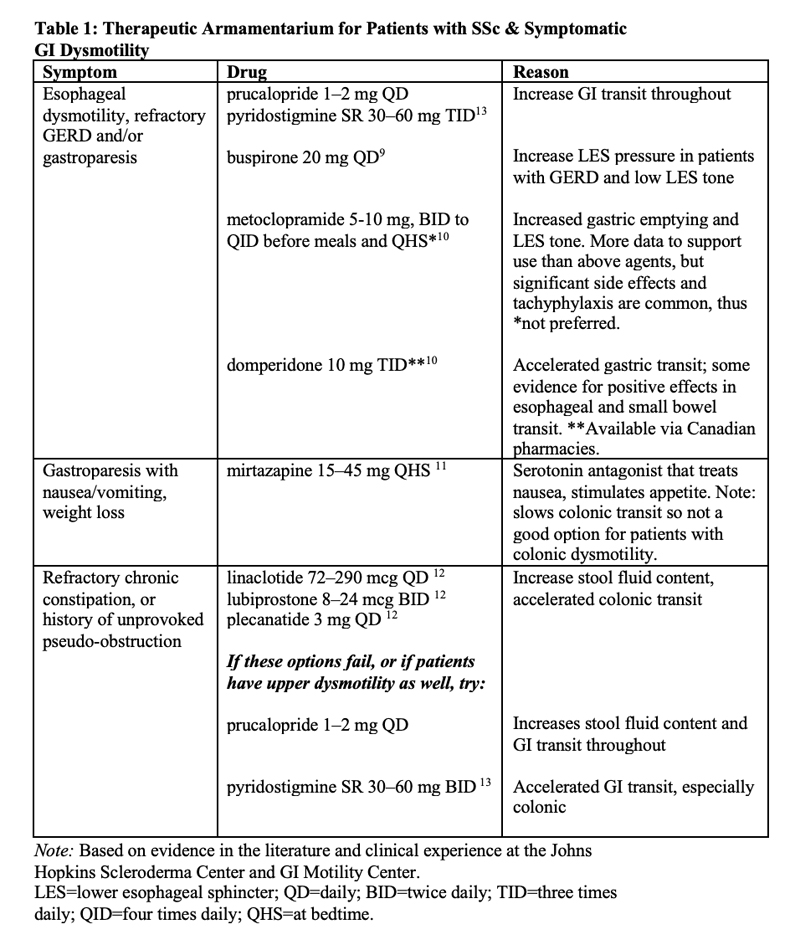
For refractory chronic constipation and in patients with a prior history of unprovoked pseudo-obstruction, motility agents, such as linaclotide, prucalopride and plecanatide, address slow colonic transit. Pyridostigmine and domperidone—available in Canada—accelerate overall GI transit, so they could be good choices for patients with multi-level GI lesions [Table 1].
TR: Is whole gut transit scintigraphy widely available?
Dr. McMahan: Currently, it’s only available at select academic centers. My hope is that research like ours will lead to more widespread availability down the line. Of note, the SmartPill motility capsule is much more widely available and correlates pretty well with whole gut transit scintigraphy.8
TR: Do you have any tips for our readers on insurance approval, especially when it comes to more expensive prokinetic or chronic constipation therapies?
Dr. McMahan: The best advice I can give is to document every single drug failure in a note, including over-the-counter options, such as polyethylene glycol or Smooth Move tea. Studies like ours can also be referenced in letters of appeal and peer-to-peer reviews.
TR: Where would you like to see research go from here?
Dr. McMahan: For starters, I’d like to be able to better risk-stratify patients. For a high-risk progressor, perhaps early therapy could prevent progression. For a person at low risk, we could take the burden of worry away and eliminate unneeded GI referrals and tests.
Next, I’d like to better understand the actual biological mechanisms that are driving GI disease in SSc. That way, we can develop treatments that don’t just target symptoms, but prevent or stop disease.
And finally, I’d like to see clinical trials look at combination therapies that target both symptoms and physiologic dysfunction. For example, would combining a promotility agent with antacid therapy at baseline in high-risk subgroups be more helpful than focusing on amplifying antacid doses alone?
Conclusion
For years, we’ve had limited treatment options for GI disease in our SSc patients. McMahan et al. have taken pivotal steps to changing that paradigm. With better knowledge about the exact location of GI involvement, we can hope for personalized therapies for symptom relief or, better yet—prevention and cure—in the future.
Samantha C. Shapiro, MD, is an academic rheumatologist and an affiliate faculty member of the Dell Medical School at the University of Texas at Austin. She received her training in internal medicine and rheumatology at Johns Hopkins University, Baltimore. She is also a member of the ACR Insurance Subcommittee.