NEW YORK (Reuters Health)—Using tumor necrosis factor alpha (TNF-alpha) inhibitors for atypical dermatoses may unmask, or perhaps even worsen, cutaneous lymphoma, according to new research.
“Our findings suggest that careful skin examination might be required in all patients prescribed anti-TNF-alpha agents, especially those with atypical presentations of benign skin conditions,” says Dr. Joan Guitart of Northwestern University Feinberg School of Medicine in Chicago. She recommended that these patients undergo skin biopsy plus specific peripheral blood work-up.
“When a skin lymphoma cannot be completely ruled out, physicians should consider alternative therapies or closely monitor patients after the start of anti-TNF-alpha treatment,” Dr. Guitart tells Reuters Health by email.
For the study, online Jan. 4 in the Journal of the American Academy of Dermatology, Dr. Guitart and colleagues did a chart review for patients diagnosed with cutaneous lymphoma at their institution after initiation of anti-TNF-alpha therapy and also reviewed the literature.1
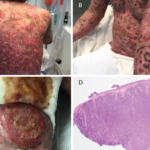
They identified 22 patients (15 male and seven female); 18 had a skin disorder prior to treatment and 15 had a biopsy. The most common histologic findings, seen in 10 patients, were psoriasis or psoriasiform dermatitis.
After treatment with anti-TNF-alpha, 20 (90%) patients were diagnosed with cutaneous T-cell lymphomas and two (9%) with indolent cutaneous B-cell lymphomas. Mycosis fungoides and Sezary syndrome were the most common subtypes of cutaneous T-cell lymphoma.
For 15 patients (75%), the indication for anti-TNF-alpha therapy was a presumed inflammatory skin disorder, most commonly psoriasis, psoriasiform dermatitis, or idiopathic erythroderma.
Five (25%) patients were diagnosed with either rheumatoid arthritis, Crohn’s disease, or sarcoidosis; three of these had a concomitant but unspecified dermatitis prior to the start of immunosuppressant therapy.
The median time from the start of anti-TNF-alpha agents to the diagnosis of cutaneous T-cell lymphoma was six months (range: 1–24).
Three patients died from their cutaneous T-cell lymphoma; one did so two months after the start of anti-TNF-alpha therapy.
Both patients with cutaneous B-cell lymphoma achieved complete remission.
The literature search identified an additional 31 cases.
Twenty (65%) patients received an anti-TNF-alpha agent to treat a systemic disease (e.g., rheumatoid arthritis, irritable bowel syndrome); six had a concurrent and poorly characterized skin disorder.
Among the 17 patients with any kind of dermatosis, less than half had a biopsy prior to the start of anti-TNF-alpha treatment, or had one with inconclusive results.
“Our findings suggest that most of the identified patients were misdiagnosed as having psoriasis or eczema; therefore, a comprehensive morphological and molecular review of skin biopsies and peripheral blood should be considered prior to initiation of anti-TNF-alpha therapy in patients with poorly defined dermatitis or atypical presentations of “psoriasis”,” the researchers write.