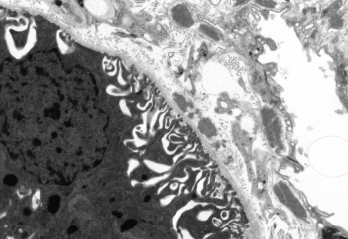
Patricia Navarro, Roger J. Bick, Brian J. Poindexter / UT-Houston Medical School/Science Source
Over time, systemic lupus erythematosus (SLE) can lead to considerable organ damage. Preventing this outcome is complicated by a scarcity of treatment options that can drive the disease into remission and by the side effects of existing therapies, such as prednisone and other corticosteroids, which may themselves contribute to the long-term damage.
The largest study to date comparing remission with lupus low disease activity state (LLDAS) as a predictor of organ damage has found that even a small percentage of time spent in clinical remission can give patients significant protection against organ damage.1 For patients who achieve the easier target of LLDAS for at least half the time on clinical follow-up, the risk of organ damage can still be cut in half.
An Achievable Goal
Lead author Michelle Petri, MD, MPH, director of the Hopkins Lupus Center and a professor of medicine at Johns Hopkins University School of Medicine, Baltimore, says her study reaffirms the clear benefits of remission while backing a more realistic treat-to-target strategy for rheumatologists. “Our current therapies just are not good enough to achieve remission. LLDAS offers an achievable outcome that will push us to treat to target,” Dr. Petri says. “LLDAS is easy to complete: It should be doable in the routine clinic setting and not overly burdensome to the rheumatologist in practice.”
Two independent rheumatologists say they agree with the study’s main conclusions. Ronald van Vollenhoven, MD, PhD, director of the Amsterdam Rheumatology and Immunology Center in the Netherlands, says he “really liked the study” and agrees that because LLDAS is more easily achievable and confers significant health benefits, it offers a reasonable outcome target.
“Having said that, both patients and expert physicians agree that, in the end, remission is desirable,” says Dr. van Vollenhoven, who is also chief of the Department of Rheumatology and Clinical Immunology at the Academic Medical Center and of the Department of Rheumatology at Vrije Universiteit Medical Center, Amsterdam. “Perhaps the two goals or targets could be combined in a long-term treatment strategy [in which] the patient is hopefully able to achieve LLDAS as a first step—and then move on to remission.”
Eric Morand, PhD, FRACP, head of the School of Clinical Sciences and a rheumatologist at Monash University’s Monash Health in Melbourne, Australia, likewise agrees with the study’s conclusions and notes that several other published clinical trials and abstracts have supported the attainability of treating to target for LLDAS. “Remission of course remains the goal, but just as in rheumatoid arthritis, it took both good measures and breakthrough medicines to establish remission as a feasible goal for usual care,” Dr. Morand says. “For now, LLDAS has the data behind it.”
Study Details
The study, published recently in Arthritis & Rheumatology, assessed data from 1,356 patients who had been followed quarterly within the Hopkins Lupus Cohort and who accounted for 77,105 person-months of observation from 1987 to 2016. In 13% of those person-months, the patient achieved clinical remission with no treatment, while 27% achieved clinical remission on treatment. By far the largest category, though, was LLDAS, which was reached in 50% of all person-months.
Patients who were in the clinical-remission-on-treatment category at any point in time—even for less than 25% of their follow-up—reduced their rates of organ damage by nearly half. Spending at least half of the time in the LLDAS category offered a comparable reduction in overall organ damage. Interestingly, this latter achievement offered protection only against certain kinds of damage, such as osteoporotic fractures, myocardial infarctions and musculoskeletal, central nervous system and renal damage. Strikingly, it did not prevent malignancies, cataracts, pulmonary fibrosis, pulmonary hypertension or cognitive impairment.
“I was surprised that LLDAS does not protect against all kinds of organ damage, such as malignancy and cognitive impairment. There is still so much to learn,” Dr. Petri says. “Pulmonary hypertension might be mediated by antiphospholipid antibodies rather than disease activity or prednisone.” The lack of an effect on pulmonary fibrosis, she adds, remains a puzzle.
“It is likely that different pathophysiological processes are behind the syndrome we call lupus, and these may lead to different long-term consequences,” Dr. van Vollenhoven says. One potential explanation for the findings, he says, is that the processes behind the specific consequences seen among the LLDAS patients hadn’t fully switched off.
Dr. Morand, though, cautioned against overanalyzing the differences in organ damage protection until they’ve been confirmed in other patient cohorts. “The prevalence of various adverse outcomes varies with race, age, gender and treatment, and we don’t know for sure if this finding will be reproduced,” he says. A reduction in cardiovascular damage, in particular, has been highly sought after for SLE patients. “It is likely to result in improved survival, but it is too early to make such a conclusion,” Dr. Morand says.
Like other studies, Dr. Petri’s clinical research found substantially more disease activity in African-American patients, and she stresses the importance of reporting results in different ethnicities because lupus is more severe in both African Americans and Hispanics. Yet her study also suggests that if they can achieve remission or LLDAS, African-American patients have reduced rates of organ damage as well, meaning the outcome category is valid in multiple ethnicities and, thus, generalizable.
Steroids Work—& Hurt
Given the role of corticosteroids in heightening the danger of long-term damage, the study may aid efforts to continue parsing the benefits and risks of low and moderate doses. Clinical remission on treatment, for example, allows up to 5 mg of prednisone per day, whereas LLDAS allows up to 7.5 mg. Dr. Petri says her research group previously found that a 6 mg daily dose of corticosteroids is the upper cutoff for avoiding organ damage: doses above that amount, she says, increase permanent organ damage by 50% or more.
“We are stuck with steroids in lupus; they work and they work fast,” Dr. Petri says. “We just cannot maintain them long term at 6 mg or more.”
Other research by her group suggested that durable remission is rare among SLE patients, supporting her study’s position that LLDAS is a more reachable goal for a treat-to-target strategy.2 She agrees with Dr. Morand and Dr. van Vollenhoven that a clinical trial will be needed to confirm whether such an approach is in SLE patients’ best interests. “But now, at least, we have the target,” Dr. Morand says.
Bryn Nelson, PhD, is a medical journalist based in Seattle.
References
- Petri M, Magder LS. Comparison of remission and lupus low disease activity state in damage prevention in a United States systemic lupus erythematosus cohort. Arthritis Rheumatol. 2018 May 27. [Epub ahead of print]
- Wilhelm TR, Magder LS, Petri M. Remission in systemic lupus erythematosus: durable remission is rare. Ann Rheum Dis. 2017;76:547–553.



