 With the U.S. Food & Drug Administration’s approval in 2014 of asfotase alfa for replacement of tissue-non-specific alkaline phosphatase (TNSALP or TNAP) in juvenile-onset hypophosphatasia (HPP), rheumatologists have a responsibility to recognize the more subtle manifestations of this condition in adults to avoid missed treatment opportunities for fractures, dental loss and musculoskeletal pain.
With the U.S. Food & Drug Administration’s approval in 2014 of asfotase alfa for replacement of tissue-non-specific alkaline phosphatase (TNSALP or TNAP) in juvenile-onset hypophosphatasia (HPP), rheumatologists have a responsibility to recognize the more subtle manifestations of this condition in adults to avoid missed treatment opportunities for fractures, dental loss and musculoskeletal pain.
Hypophosphatasia is a heterogenous disorder deriving from more than 400 known mutations in the alkaline phosphatase gene (ALPL), presenting in both children and adults with persistently low alkaline phosphatase levels and associated abnormalities that vary widely—from osteomalacia and fractures to chondrocalcinosis and (sometimes exclusively) abnormalities of dental mineralization or premature tooth loss. The shared deficits in affected individuals relate to an impact of loss-of-function mutations in the tissue non-specific alkaline phosphatase enzyme responsible for manufacturing inorganic phosphate from pyrophosphate for incorporation into bone matrix, with additional impact on vitamin B6 metabolism resulting in difficulty transporting B6 from the blood into the central nervous system.1
Prevalence & Diagnosis
Hypophosphatasia is a rare condition: Estimates of the prevalence of severe disease in children range from 1 in 100,000 to 1 in 300,000, and the prevalence of milder disease is presumed to be higher in adults but is not yet informed by reliable population-based data.2
The condition must be distinguished from more common causes of persistently low alkaline phosphatase, including nutritional deficiencies, celiac disease, hypothyroidism and hypoparathyroidism, bisphosphonate use, chemotherapy and adynamic renal osteodystrophy.3
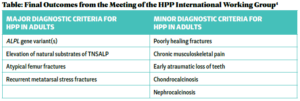
Recent proposed diagnostic criteria by the HPP International Working Group for patients with persistent hypophosphatemia include four major and nine minor criteria—of which two major, or one major and two minor criteria must be present (see Table).4 These criteria have not yet been validated but represent the first consensus guidelines for diagnosis in both pediatric and adult populations.
Musculoskeletal Signs & Symptoms
Importantly for rheumatologists, musculoskeletal signs and symptoms are common among adults with hypophosphatasia. In one review, the pooled prevalence of musculoskeletal symptoms was high, including 64% of patients with chronic musculoskeletal pain, 64% with poorly healing fractures, 39% with recurrent metatarsal stress fractures and 16% with chondrocalcinosis or calcium pyrophosphate deposition disease. Overall, the prevalence of dental abnormalities included early loss of primary teeth in 34% and loss of secondary teeth without periodontal disease in 5%.4
Ligamentous calcium hydroxyapatite deposition is another consequence of the disordered inorganic phosphate handling, resulting in calcific enthesopathy and diffuse idiopathic skeletal hyperostosis.5
Treatment & Testing
In general clinical practice, persistently low alkaline phosphatase is the most readily available initial test—with recognition that acute fractures can temporarily normalize or increase alkaline phosphate levels—that should prompt an initial clinical assessment for evidence of increased fractures or osteomalacia, derangements in calcium and phosphate handling, such as chondrocalcinosis, hypercalcemia, nephrocalcinosis and dental abnormalities.
Phosphate levels tend to be high or normal in hypophosphatasia and help distinguish this from X-linked hypophosphatemia, in which phosphate levels are characteristically low.
Measurement of tissue pyridoxal 5-phosphate (the dominant form of vitamin B6 reported by most commercial labs) and urine phosphoethanalomaine (PEA) levels are sensitive screening tests, elevated in about 90% of patients, that help distinguish hypophosphatasia from other contributors to metabolic bone disease, although urine PEA is not readily available through the most common commercial labs.4
Genetic confirmation of ALPL gene mutations is now commercially available through Labcorp, Invitae and Prevention Genetics.
Once identified, treatment involves serial assessment and management of calcium, phosphate and magnesium levels; treatment of associated pseudogout and diffuse idiopathic skeletal hyperostosis (DISH) with non-steroidal anti-inflammatory drugs and usual symptomatic management, and treatment of fractures with surgical management. For symptomatic patients, injection with asfotase alfa (human TNSALP) is indicated. The recommended dose for adults is the same as for children, 2 mg/kg subcutaneously three times weekly.
Vitamin D, phosphate and calcium levels should be monitored serially due to the risk of a hungry bone phenomenon, although use of high-dose ergocalciferol and calcitriol has been discouraged due to a higher risk of hypercalcemia in these patients. Data regarding effectiveness of asfotase alfa for symptoms in adults is early and limited to case series, but preliminary reports note improvements in pain, mobility and quality of life.6
Bisphosphonates are generally avoided in both child and adult populations because they can theoretically worsen fracture risk due to their resultant reduction in availability of magnesium and zinc cofactors, and they compete with already decreased inorganic phosphate for incorporation into bone.7 If baseline alkaline phosphatase levels are not obtained before treatment, bisphosphonates can erroneously be presumed the cause of the low alkaline phosphatase levels.
 Colin Ligon, MD, MHS, is a clinical rheumatologist with Penn Specialty Practices Pottstown, Pennsylvania. He is an associate editor of The Rheumatologist.
Colin Ligon, MD, MHS, is a clinical rheumatologist with Penn Specialty Practices Pottstown, Pennsylvania. He is an associate editor of The Rheumatologist.
References
- Michigami T, Ohata Y, Fujiwara M, et al. Clinical practice guidelines for hypophosphatasia. Clin Pediatr Endocrinol. 2020;29(1):9–24.
- Whyte MP. Hypophosphatasia—Aetiology, nosology, pathogenesis, diagnosis and treatment. Nat Rev Endocrinol. 2016 Apr;12(4):233–246.
- Khan AA, Brandi ML, Rush ET, et al. Hypophosphatasia diagnosis: Current state of the art and proposed diagnostic criteria for children and adults. Osteoporos Int. 2024 Mar;35(3):431–438. Erratum in: Osteoporos Int. 2024 May;35(5):933–934.
- Brandi ML, Khan AA, Rush ET, et al. The challenge of hypophosphatasia diagnosis in adults: Results from the HPP International Working Group Literature Surveillance. Osteoporos Int. 2024 Mar;35(3):439–449. Erratum in: Osteoporos Int. 2024 May;35(5):933–934.
- McKiernan FE, Berg RL, Fuehrer J. Clinical and radiographic findings in adults with persistent hypophosphatasemia. J Bone Miner Res. 2014 Jul;29(7):1651–1660.
- Kishnani PS, Martos-Moreno GÁ, Linglart A,et al. Effectiveness of asfotase alfa for treatment of adults with hypophosphatasia: Results from a global registry. Orphanet J Rare Dis. 2024 Mar 8;19(1):109.
- Bianchi ML, Bishop NJ, Guañabens N, et al.; Rare Bone Disease Action Group of the European Calcified Tissue Society. Hypophosphatasia in adolescents and adults: Overview of diagnosis and treatment. Osteoporos Int. 2020 Aug;31(8):1445–1460.