ldutko/shutterstock.com
WASHINGTON, D.C.—As treatments for rheumatoid arthritis (RA) improve, some related conditions that used to be common in patients with RA are not seen very often anymore, but they still exist and physicians need to know how to identify them.
Speaking to attendees at the ACR/ARHP Annual Meeting talk titled Rheumatoid Arthritis—A Case-Based Approach to Selected Extra-Articular Challenges and What You Are Missing with Better Therapies, part of the ACR Review Course, expert Jonathan Coblyn, MD, director of clinical rheumatology at Brigham and Women’s Hospital in Boston, outlined several clinical cases to support his main message. He reviewed cases involving several conditions that newer treatments have made fairly rare: central nervous system (CNS) manifestations of RA, cervical spine involvement, Felty’s syndrome and large granular lymphocyte (LGL) leukemia.
CNS Manifestations in RA
This case involved a 71-year-old man with a long history of RA and pulmonary fibrosis who has been on azathioprine and received a yearly rituximab injection. Two months before being admitted, he’d developed persistent hiccups. A chest X-ray led to treatment of community-acquired pneumonia, after which he did better. But the symptoms returned, and he came back two weeks later with the hiccups again, had lost 30 lbs. and couldn’t swallow liquids or solids.
CNS manifestations of RA include CNS vasculitis; rheumatoid nodules; sterile meningitis and pachymeningitis; infections, including progressive multifocal leukoencephalopathy (PML); hyperviscosity syndromes; cerebrovascular disease; CNS tumors or lymphoma; and effects of medication.
PML has to be a consideration when a patient is on rituximab, but involves neuroimaging that is distinct, meaning that it is limited to the white matter and doesn’t conform to vascular areas as vasculitis would, Dr. Coblyn said. The man was transferred to Brigham and Women’s Hospital.
“He had hiccups that were persistent; that was our clue,” Dr. Coblyn said. A neurologist said that whenever hiccups are involved, attention should be paid to the area postrema, a region in the dorsal surface of the medulla oblongata that lacks the blood–brain barrier and can detect emetic toxins in the brain and the blood. By examining the findings of his magnetic resonance imaging test, they determined that the man had significant inflammation in the area postrema. More studies were done, including flow cytometry of the cerebrospinal fluid, and the man was given broad-spectrum antibiotics and antifungals.
But—as often happens in these cases, Dr. Coblyn said—the diagnosis was made at autopsy. Neuropathology eventually found he had diffuse large B-cell lymphoma, with “notable involvement of basilar leptomeninges by [Epstein-Barr] EBV-virus lymphoma.”
It’s possible, Dr. Coblyn said, the rituximab treatment could have obscured or delayed the diagnosis, but it’s unknown whether that was the case.
Cervical Spine & RA
This case involved a 55-year-old woman with longstanding RA and increasing knee pain. On examination, she also had numbness in her hand, which worried an orthopedics colleague, so the patient had spine film X-rays with flexion and extension views.
Neurologic manifestations of RA that don’t involve the CNS include entrapment neuropathies, peripheral neuropathies, rheumatoid nodules and mononeuritis multiplex.
The patient’s X-rays showed a “dramatic” separation between the anterior arch of C1 and the odontoid process, which is evidence of subluxation of the C1 and C2 vertebrae (C1–2).
Clues for C1–2 subluxation include upper or lower extremity numbness, C2–3 radicular pain and brainstem symptoms, such as drop attacks, dysphagia or vertigo. But there may be no symptoms.
“You really need to have a high index of suspicion,” Dr. Coblyn said. “Don’t wait for symptoms.”
A difficult question in these cases is whether to intervene. A C1–2 distance of more than 8 mm is often a sign to intervene. But the posterior atlanto-odontoid interval might be a better indicator of whether to do surgery: A distance of less than 14 mm is often used as a cut-off, Dr. Coblyn said.
Dr. Coblyn mentioned one study that showed dramatically different results for surgery and non-surgery.1 Nineteen patients with cervical lesions caused by RA were treated with surgery at one hospital, and 21 others were treated without surgery at another. The survival rate for the surgery group was 84% at five years and 37% at 10 years. The non-surgery group showed worsening of neurologic symptoms in 76%. All were bed-ridden at three years, and all had died by eight years.
“This, I think, is a pretty powerful suggestion that if you have someone with these conditions with myelopathy and C1–2 subluxation and/or basilar invagination (a folding-in of the skull base when the C2 vertebra migrates upward), you probably want to go ahead and do that surgery,” said Dr. Coblyn.
Felty’s syndrome & LGL in RA
Felty’s syndrome—a combination of RA, enlarged spleen and low white blood cell count—can be a precursor to LGL syndrome in RA. Dr. Coblyn said 85–90% of patients with RA and LGL are seropositive for HLA-DR4. RA in those with Felty’s and LGL tends to present later and have a more benign course than those presenting with de novo LGL.
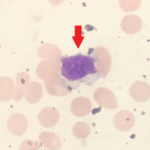
A diagnosis of LGL usually involves leucopenia, but not always. The LGL cells are typically seen in a peripheral smear or bone marrow, he said. Most likely, Felty’s is a polyclonal LGL syndrome, which becomes an LGL diagnosis when it becomes monoclonal, Dr. Coblyn noted.
In this case, a 65-year-old woman with a history of seropositive, erosive RA had tried a variety of treatments without much response, but then was diagnosed with Felty’s syndrome after increased leucopenia. The initial treatment included high-dose prednisone and cyclic cyclophosphamide, on which she did better. But the anemia and leucopenia continued.
Her RA got worse and Dr. Coblyn said he suggested using rituximab for both her RA and her LGL. Since then, the therapy has been effective.2
“We ended up collecting in-house about seven patients with RA and LGL, all treated with rituximab,” he said. “And virtually all of them did excellently in terms of their LGL, and most of them with their RA.”
RA & Vasculitis
Dr. Coblyn said physicians need to be aware of vasculitis in patients with seropositive RA using steroids, often without disease-modifying anti-rheumatic drugs, who present with skin lesions or mononeuritis multiplex, among other manifestations.
Treatment may include steroids and immunosuppressive drugs. And the literature is growing on the use of rituximab.
Thomas R. Collins is a freelance writer living in South Florida.
References
- Matsunaga S, Sakou T, Onishi T, et al. Prognosis of patients with upper cervical lesions caused by rheumatoid arthritis: Comparison of occipitocervical fusion between c1 laminectomy and nonsurgical management. Spine (Phila Pa 1976). 2003 Jul 15;28(14):1581–1587.
- Cornec D, Devauchelle-Pensec V, Jousse-Joulin S, et al. Long-term remission of T-cell large granular lymphocyte leukemia associated with rheumatoid arthritis after rituximab therapy. Blood. 2013 Aug 29;122(9):1583–1586.