Laboratory analysis revealed an elevated creatinine to 1.7 and PUA of 9.6 mg/dL.
Hand X-rays from three years prior were notable for severe polyarticular erosive disease. Plain films obtained in our institution confirmed multiple erosions involving the MCP, DIP and PIP joints, overlying soft tissue masses containing amorphous calcifications, loss of cartilage in the intercarpal bones, and carpal bony erosions. Plain films of the elbows and ankles similarly revealed large amorphous deposits and calcifications. Multiple erosions were also present at the first metatarsal head, tarsometatarsal joints and at the bases of the metatarsal and intertarsal joints.
(click for larger image)
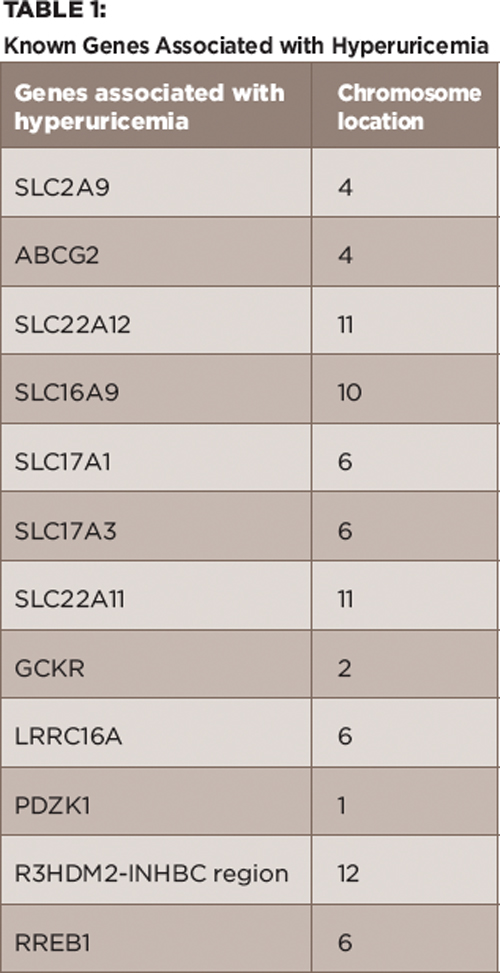
Table 1:
Known Genes Associated with Hyperuricemia
At that time, treatment with febuxostat was initiated at 40 mg/day, which was gradually increased to 120 mg/day with limited results. Initially, the patient noted a slight improvement in the frequency of his gout flares, but soon he began having recurrent flares, as before. He started to require frequent prednisone bursts and, ultimately, ended up using low-dose prednisone as prophylaxis. His PUA was monitored every three months during this period, and he remained in the range of 9–10 mg/dL.
Given his treatment failure with febuxostat, the decision was made to start pegloticase. Prior to initiating this treatment, a new set of plain films was obtained, which showed progression of tophi, as well as new erosions in multiple sites involving his hands, elbows, feet and ankles.
Pegloticase was administered intravenously at 8 mg every two weeks for a total of 10 infusions. In addition, he was treated with 20 mg of prednisone daily because he continued to have acute gout flare-ups on lower doses of prednisone. PUA was checked before each infusion, and the values are reported in Figure 1. After a few infusions, based on the reported PUA values, we discussed with the patient the possibility of discontinuing the infusion due to fear of an infusion reaction from antibody formation. The patient, however, accepted the risks and decided to continue the infusion.
Over the course of his five months of infusions, he subjectively reported improvement in his range of motion, as well as a decrease in the size of his tophi. However, clinically these findings were not appreciated. And although the frequency of gout flares was reduced, this was likely secondary to the prednisone more than the pegloticase itself. Unfortunately, with the exception of one value of 8.1 mg/dL at the time of the second infusion, PUA values remained elevated in his pretreatment range of 9–10 mg/dL. Overall, the infusions were well tolerated, and no hypersensitivity reactions occurred; however, we were unable to check if the patient developed antibodies against pegloticase.


