
Marcin Balcerzak / shutterstock.com
The past 20 years have seen dramatic changes in the practice of rheumatology, ranging from bench to bedside therapeutic advances to dramatic improvements in diagnostic imaging. The results have been gratifying for our patients and attractive to internal medicine trainees making subspecialty career decisions. We are pleased to provide this article for The Rheumatologist’s wide-ranging readership, from expert sonographers to those of you who regard the best use of one of these machines as a doorstop for your procedure room.
Consistent with our teaching techniques, our comments range from mostly serious to the occasionally humorous, even though we (well, at least one of us anyway) may occasionally sink to the level of a bad dad joke.
Over the past decade, more than 400 rheumatology fellows and faculty members have incorporated ultrasound use into their practice under the guidance of our group, whose diabolical methods include an eight-month blended learning program that includes remote learning, a hands-on workshop and an in-person written and practical examination at the end.1 Thanks to the proliferation of practicing rheumatologists versed in ultrasound, many rheumatology fellows are now being mentored in ultrasound imaging by their local faculty as part of their fellowship training.2 Other rheumatologists learn ultrasound through a combination of weekend workshops and self-study, but without the benefit of ongoing feedback.
After the conclusion of our most recent, sweat-filled, grueling examination, the course faculty reviewed some of the most common predicaments our students experienced to guide teaching modifications for the following year. We summarize these pitfalls now with the hope it will be of use to providers learning rheumatologic ultrasound (RhUS), as well those of you who remain uncertain about its relevance. The discussion is subdivided by joint region, so the discussion does not become disjointed (pun with apologies from Paul DeMarco [PD]).
General Comments
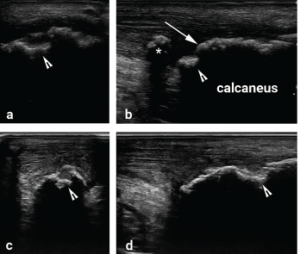
Figure 1
Images a and b were obtained from the posterior heel by one student and c and d by another student from the same model patient on the same day. The erosion is much better defined on both longitudinal and transverse views in c and d, while it is harder to distinguish erosion from osteophyte on images a and b. An erosion (arrowhead) is noted on all views. A normal calcaneal surface (arrow) that could be mistaken for an osteophyte if the erosion next to it were not recognized as an erosion. On image b, there is tendon calcification (asterisk) that is not demonstrated in the other views. These images show the importance of sweeping the transducer through the entire width of the target structure to avoid missing pathology, and the need to correlate longitudinal and transverse images to define abnormalities.
When performing a RhUS examination, it’s critical to sweep the transducer across the entire target structure, or asymmetrically located pathologies (e.g., swollen synovium, effusion, erosion) may be missed.
On our practical exam, only a minority of students performed thorough scanning through the target tissues, instead focusing on getting a perfect image in one plane (see Figure 1). This may have partially been due to time pressure, the grading scheme for the exam or the intimidating poker face of our exam proctors, but scanning through the entire region of the target tissue is, in any case, an important teaching point to emphasize.
Students of RhUS should learn to scan using light transducer pressure, except when pressing/compressing helps differentiate hypoechoic (low sound reflection/dark) or anechoic (no sound reflection/black) tissue from effusion. Although most students scan with light pressure, few routinely use more compression to help make this distinction. Some also assume that all anechoic tissue without Doppler signal indicates fluid collection, forgetting that hyaline cartilage, anisotropy (the artifact occurs when sound waves strike mirror-like reflective tissues, such as tendons at non-perpendicular angles and are reflected away from the transducer surface, resulting in an abnormally dark image), edematous synovium and machine setting imperfections all can result in tissue appearance similar to that of synovial fluid (anechoic) (see Figure 2).


