“This is a clear failure of that immune checkpoint,” she said. Erythrocyte sedimentation rate testing can show that PD-L1 expression on dendritic cells inversely correlates with inflammatory markers in GCA patients. When researchers treated bio-engineered mice with a checkpoint inhibitor to block PD-L1, “we see that it breaks the immune tolerance of the vessel wall.3 If we break the checkpoint with this treatment, we get vigorous GCA disease in these arteries. Checkpoint inhibition also accelerates inflammatory cytokine production.” Treatment raises PD-1 levels, increases pro-inflammatory transcription factors, and enhances IFN-γ, IL-17A and IL-21, she said. It also unleashes T cell immunity, thickens the intima and dramatically increases microvascular angiogenesis in the adventitia.
Tocilizumab, an IL-6 inhibitor, is approved by the U.S. Food & Drug Administration to treat GCA, but unanswered questions, including whether biomarkers for disease activity are lost after therapy blocks IL-6 & if the tissue-protective functions of acute phase proteins are also blocked by treatment, are important for GCA patients, said Dr. Weyand.
Diagnosis & Therapy
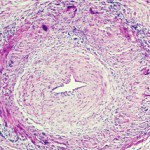
To diagnose GCA, rheumatologists typically evaluate the temporal artery, especially in patients with cranial manifestations, said Tanaz A. Kermani, MD, MS, FACP, assistant professor of medicine and director of the Vasculitis Program at the University of California, Los Angeles. Biopsy may detect disease symptoms even weeks after treatment is initiated, but it is invasive, she said. High-resolution magnetic resonance imaging (MRI) of scalp arteries shows some promise as an alternative non-invasive modality for initial GCA diagnosis, and ultr

Dr. Kermani
asound may also be helpful, but the sensitivity of both MRI and ultrasound diminish after patients start treatment.4
A new approach being studied is the fast-track clinic, where rheumatologists promptly evaluate any patients with suspected GCA, including use of ultrasound.5 If GCA is indicated, patients begin treatment right away, said Dr. Kermani. Data from these clinics has shown a dramatic decrease in vision loss, but more prospective data is needed on this approach, she said.
In evaluation, rheumatologists may overlook GCA’s possible extracranial manifestations, such as large artery stenosis or aortic involvement, said Dr. Kermani. Physical examination has poor sensitivity in diagnosing large-vessel vasculitis, so angiography or positron emission tomography (PET) may be used to find lesions in these vessels.6,7
Careful evaluation is important, because a significant portion of GCA patients may develop large-vessel manifestations, especially aortic aneurysms even 10 years after diagnosis.8
“This is an important implication for our patients. They may no longer be following up with rheumatology because they may be off treatment, but this is a late complication of the disease,” she said.