Patients with upper-extremity limb claudication may be younger than others with GCA, who have more typical cranial manifestations.9 Their diagnosis may be delayed because they lack the more common signs of GCA, said Dr. Kermani. “Maybe physicians don’t recognize it or think about it early enough. Inflammation may be in different segments, so they tend to have less vision loss,” she said. These GCA patients may have a negative temporal artery biopsy. “So if you suspect this diagnosis, large-vessel imaging is really the way to proceed in terms of your diagnostic evaluation.”
Although GCA patients should be screened for aortic aneurysms, a late-stage complication, there is no consensus on the type of imaging modality or frequency and timing of screening in these patients, she said. GCA patients are also at increased risk for vertebrobasilar stroke, myocardial infarction and venous thromboembolism, so GCA screening may be considered in older patients who present with these vascular events.10
Glucocorticoids have been the mainstay of GCA therapy in the past, and “prompt treatment in anyone with suspected GCA is essential to prevent vision loss. In patients where vision loss does occur, prompt institution of glucocorticoids can prevent contralateral eye involvement or progression of their visual deficit,” said Dr. Kermani. After a starting dose of 40–60 mg/day for one month, if symptoms resolve and biomarkers normalize, patients may taper their glucocorticoid dose. Patients with vision loss or ischemic complications such as limb claudication may need pulse steroids, she added. Aspirin is not routinely recommended.
Tocilizumab may help GCA patients lower their overall steroid dose and decrease relapse risk, according to the results of a Phase III, randomized clinical trial.11 Other potential therapies now in clinical trials include abatacept and ustekinumab, but these are not yet approved for GCA, she said.12,13
Imaging Strengths & Limitations
Rheumatologists must select the right imaging modality at different points in the GCA disease process, said Peter C. Grayson, MD, MSc, Principal Investigator of the translational research program in vasculitis at the National Institutes of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) of the National Institutes of Health (NIH). Ultrasound of extracranial vessels to diagnose GCA has many advantages, he said.14 It is relatively cheap, non-invasive, involves no radiation and can be performed at bedside.
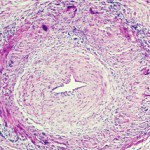
“It’s a dynamic form of imaging. You can see how blood is flowing through the arteries and see signs of turbulence,” said Dr. Grayson. “The other thing you can see in ultrasound is the wall of the artery and the morphology of it. Is this imaging finding telling me that inflammation is going on in this vessel wall? What you will see, particularly in the cross-sectional view, is you can see this hypo-echoic rim around the lumen of the artery, which is what we call the halo sign. This tells me that there is likely this edematous, thickened arterial wall,” a sign of potential arteritis.