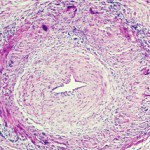
Ultrasound and temporal artery biopsy show widely variable rates of specificity and sensitivity for GCA diagnosis in different studies to compare them, Dr. Grayson said. Patients may have a normal ultrasound, but later be diagnosed with GCA. In a 2016 study comparing the two methods, ultrasound showed 81% specificity but 54% sensitivity for diagnosis of GCA, while biopsy showed 100% specificity but only 39% sensitivity.15 Both ultrasonographers reviewing scans and pathologists reviewing biopsy results may disagree on these findings in GCA, he added.
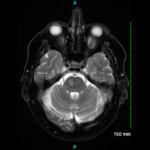
High-resolution scalp MRA can show abnormalities, such as increased wall thickness in temporal arteries, and has 80% agreement with biopsy, but many patients with a normal MRA still go on to be diagnosed with GCA.4 Fluorodeoxyglucose (FDG) PET scans cannot detect temporal artery inflammation, as the resolution of these scanners is not yet good enough for the job, he said. FDG-PET may be used to examine larger arteries like the aorta, along with angiography, said Dr. Grayson.
Both MR- and CT-based angiography platforms are non-invasive and useful for assessing disease activity and monitor GCA patients for silent disease progression. However, it is hard to cover the whole body in one session, specificity is lacking, and cost, radiation and potential adverse effects to the patient are valid concerns.
Weaknesses: It’s hard to cover the whole body in one session. Technical expertise is required for these modalities, he said.
Because it uses glucose, PET may detect metabolic activity in the walls of large arteries that suggest inflammation. PET may be used to categorize the extent of disease and assess disease activity in GCA patients, as well as monitor for silent progression of disease and, possibly, treatment response. However, these tests are hard to obtain, he said. Other limitations include a lack of a gold standard for PET’s use as a diagnostic tool in GCA, as well as cost and the use of radiation. It cannot be used to correctly assess the temporal arteries. While a 2015 meta-analysis of FDG-PET to diagnose GCA showed both high specificity and sensitivity, selection bias may have elevated those numbers, he said.16 At this time, it seems that all available imaging modalities have a role to play in diagnosis and ongoing assessment of GCA patients.
Susan Bernstein is a freelance journalist based in Atlanta.
References
- Wen Z, Shimojima Y, Shirai T, et al. NADPH oxidase deficiency underlies dysfunction of aged CD8+ Tregs. J Clin Invest. 2016;126(5):1953–1967.
- Wen Z, Shen Y, Berry G, et al. The microvascular niche instructs T cells in large-vessel vasculitis via the VEGF-Jagged-1-NOTCH pathway. Sci Transl Med. 2017 Jul;399(9):eaal3322.
- Zhang H, Watanabe R, Berry GJ, et al. Immunoinhibitory checkpoint deficiency in medium and large vessel vasculitis. PNAS. 2017;114(6):E970–E979.
- Rheaume M, Rebello R, Pagnoux C, et al. High-resolution magnetic resonance imaging of scalp arteries for the diagnosis of giant cell arteritis: Results of a prospective cohort study. Arthritis Rheumatol. 2017 Jan;69(1):161–168.
- Patil P, Williams M, Maw WW, et al. Fast track pathway reduces sight loss in giant-cell arteritis: results of a longitudinal observational cohort study. Clin Exp Rheumatol. 2015 Mar–Apr;33:(2 suppl 89):S-103–106.
- Grayson PC, Tomasson G, Cuthbertson D, et al. Association of vascular physical examination findings and arteriographic lesions in large vessel vasculitis. J Rheumatol. 2012 Feb;39(2):303–309.
- Prieto-Gonzalez S, Arguis P, Cid MC. Imaging in systemic vasculitis. Curr Opin Rheumatol. 2015 Jan;27(1):53–62.
- Kermani TA, Warrington KJ, Crowson CS, et al. Large-vessel involvement in giant cell arteritis: A population-based cohort study of the incidence-trends and prognosis. Ann Rheum Dis. 2013 Dec;72(12):1989–1894.
- Muratore F, Kermani TA, Crowson CS, et al. Large-vessel giant cell arteritis: A cohort study. Rheumatology (Oxford). 2015 Mar;54(3):463–470.
- Amiri N, De Vera M, Choi HK, et al. Increased risk of cardiovascular disease in giant cell arteritis: A general population-based study. Rheumatology (Oxford). 2016 Jan;55(1):33–40.
- Stone JH, Tuckwell K, Dimonaco S, et al. Trial of tocilizumab in giant cell arteritis. New Engl J Med. 2017 Jul;377:317–328.
- Langford CA, Cuthbertson D, Ytterberg SR, et al. A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of giant cell arteritis. Arthritis Rheumatol. 2017 Apr;69(4):837–845.
- Conway R, O’Neill L, O’Flynn E, et al. Ustekinumab for the treatment of refractory giant cell arteritis. Ann Rheum Dis. 2016 Aug;75(8):1578–1579.
- Laria A, Lurati A, Scarpellini M. Color duplex ultrasonography findings of temporal arteries in a case of giant cell arteritis: Role in diagnosis and follow-up. Open Access Rheumatol. 2017 Mar 15:9:55–59.
- Luqmani R, Lee E, Singh S, et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): A diagnostic accuracy and cost-effectiveness study. Health Technol Assess. 2016 Nov;20(90):1–238.
- Soussan M, Nicolas P, Schramm C, et al. Management of large-vessel vasculitis with FDG-PET: A systematic literature review and meta-analysis. Medicine (Baltimore). 2015 Apr.94(14):e622.