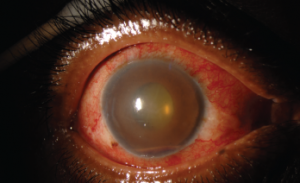
Figure 2. This external photograph of the right eye shows keratic precipitates on the corneal endothelium, corneal edema and hemorrhagic hypopyon in the setting of acute herpetic anterior uveitis.
Uveitis is an umbrella term for intraocular inflammatory diseases that can lead to vision loss. It’s not just a concern for ophthalmologists. Uveitis occurs in approximately 2–5% of patients with inflammatory bowel disease, 6–9% of patients with psoriatic arthritis and 25% of patients with reactive arthritis. The prevalence may be as high as 33% in patients with ankylosing spondylitis.1 Thus, it’s important rheumatologists have an understanding of this potentially debilitating condition.
The Basics
Sandwiched between the dense connective tissue of the sclera externally and the neurosensory retina internally, the uvea comprises the pigmented, middle layer of the eye. Composed of the iris, ciliary body and choroid, inflammation within these structures is collectively called uveitis.
The heterogeneous causes of uveitis include trauma, autoimmune disorders, infections, drug reactions and malignancies. When a cause is not identified, which occurs in approximately half of cases, the term idiopathic is used.
Intraocular inflammation is uncommon, with an estimated incidence of 26–52 cases per 100,000 people per year due to ocular immune privilege—the phenomenon in which the eye attempts to limit local immune and inflammatory responses to preserve vision.2,3 The eye lacks lymphatic drainage, and the aqueous humor contains immunosuppressive factors, including TGF-β.4 Additionally, intraocular tissues express Fas ligand, which promotes leukocyte apoptosis.4
Classifications
Intraocular inflammation is classified on the basis of anatomic location using the standardization of uveitis nomenclature (SUN):5
- Anterior uveitis accounts for 50–90% of cases of ocular inflammation.6 It refers to inflammation of the iris or ciliary body with the focus of inflammation centered in the anterior chamber. Previous terms for anterior uveitis include iritis, iridocyclitis or anterior cyclitis.
- Intermediate uveitis and posterior uveitis occurs in the posterior chamber. Intermediate uveitis describes inflammation within the vitreous body, which includes pars planitis or posterior cyclitis.
- Posterior uveitis refers to inflammation predominately in the retina or choroid, and encompasses entities such as retinal vasculitis or neuroretinitis.
- Finally, panuveitis occurs when inflammation is evenly distributed throughout the eye and not restricted to one chamber.
Uveitis can also be classified by onset or course.6 Although the onset of uveitis can be either sudden or insidious, the course denotes the duration.
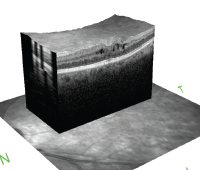
Cystoid macular edema is seen on optical coherence tomography. The hyporeflective spaces within the retina represent fluid accumulation due to inflammatory vascular leakage. This is most common cause of vision loss in patients with uveitis.
Acute uveitis describes inflammation occurring for less than six weeks with sudden onset. If inflammation resolves, treatment is stopped, but if it occurs again after three months, the uveitis is considered recurrent. If there is less than three months of inactivity and lack of a treatment-free interval between episodes of inflammation, the uveitis is considered chronic.
Uncontrolled, chronic inflammation causes structural complications leading to blindness, including macular edema, cataracts, glaucoma or neovascularization of the retina.7
As the cause of 10–15% of blindness in the U.S. and Europe, uveitis and associated complications predominately affect patients during their working years. This leads to significantly more lost wages, increased medical costs and increased rates of disability compared to age-matched peers.8-10 Thus, rapid and continued control of intraocular inflammation is required.


