Evidence from a randomized trial has supported that MTX can be used to induce remission of nonsevere WG.9 Oral or subcutaneous MTX is started at 15 mg/week (0.3 mg/kg/week) and increased within the first two to four weeks to 20–25 mg/week. To reduce toxicity, MTX is given with folic acid 1 mg daily or folinic acid 5 mg once a week taken 24 hours after MTX.
Maintenance
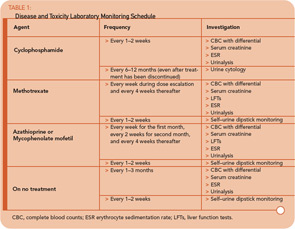
To date, there have been no comparative trials among individual maintenance agents. Therefore, a decision about which medication to use must be based on individual factors, including contraindications and relapse history. In the absence of cytopenias, the maintenance agent can be started within one to two days after stopping CYC.
For remission maintenance in WG, the largest body of data involves the use of AZA or MTX.10,11 AZA is given at a dose of 2 mg/kg/day, and MTX is given at doses as described for induction. Screening for thiopurine methyltransferase (TPMT) should be performed prior to AZA initiation when possible.
There has been a smaller body of published data with the use of mycophenolate mofetil (MMF)12 and leflunomide.13 MMF in particular may play a role in patients who cannot take AZA or MTX or those who have relapsed through these agents.
The optimal duration of maintenance therapy remains unclear. Although it is likely that relapse occurs more frequently in patients off treatment, prolonging therapy must be balanced against the potential for relapses that can still occur on medication, drug toxicity, and the ability of some patients to come off treatment. For newly diagnosed patients who do not have significant organ damage, treatment should be continued for at least two years in the absence of toxicity, after which time the clinician can consider tapering towards discontinuation. In patients who have relapsed or who have had severe permanent organ damage, treatment for a longer duration may become necessary.
Trimethoprim–Sulfamethoxazole
Because of its antimicrobial properties, the use of trimethoprim–sulfamethoxazole (T/S) for the treatment of WG has been difficult to assess. Use in isolated sinonasal disease can be considered with close observation, although it should never be used alone for other disease features. The role of T/S to reduce relapses was examined in a placebo-controlled randomized study and, although it lowered the rate of upper airways relapses, T/S did not prevent relapses in major organ sites.14