
In August 2001, Diane Endicott* noted the spontaneous onset of tightening of the skin over her feet and lower legs. Endicott was a 40-year-old woman with type 1 insulin-dependent diabetes mellitus which started at age 10 and stage 5 chronic kidney disease (kidney failure with glomerular filtration rate less than 15 mL/min/1.73 m2 or receiving dialysis), who had been on hemodialysis for the previous two years. This skin tightening progressed rapidly to involve the skin on her thighs, hands, and forearms. It also involved the skin over her breasts and in her perineal region. She observed the skin in these areas to be thickened and tethered to the underlying tissue and darker in color than her skin elsewhere.
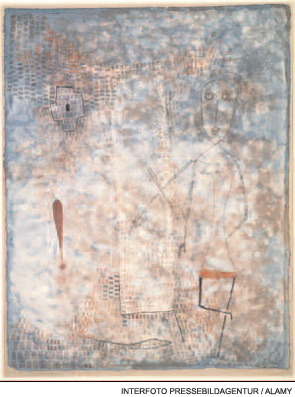
Her fingers became fixed in flexion. Her hands became claw-like, causing her difficulty buttoning her blouse, and she developed fixed flexion contractures of her knees. (See Fig. 1) Because she could not fully extend either leg, she no longer was able to walk independently and required the use of a wheelchair to move. She also developed conjunctival erythema and yellow scleral plaques. As her skin changes progressed to extend above her elbows, Endicott also developed fixed flexion contractures of her elbows and she became incapacitated by severe, burning pain in her extremities that kept her awake at night. However, she noted no tightening of the skin on her face and had never experienced color change of her digits upon cold exposure.
Endicott’s nephrologist was puzzled by the rapid onset of this scleroderma-like condition, having never seen this before among the other patients receiving dialysis under his care. To clarify Endicott’s diagnosis, he referred her to the rheumatology consultant at his hospital. The consultant had seen patients with scleroderma develop renal failure during scleroderma renal crisis. However, he, too, had never observed a patient with pre-existing stage 5 chronic kidney disease develop the new onset of cutaneous changes of scleroderma. Thus, he referred Endicott to a nearby academic medical center for dermatologic evaluation and for another rheumatologic opinion.
Early Cases
During the preceding four years, between May 1997 and November 2000, eight of 265 patients who had received renal allografts at Sharp Memorial Hospital in San Diego developed the relatively rapid onset of skin changes similar to Endicott’s and that resembled scleromyxedema. Each of these eight patients developed fibrotic skin changes on the trunk and extremities, which resulted in debilitating joint contractures. However, none developed facial involvement or had the circulating IgG lambda paraprotein that would be expected in scleromyxedema.1 Skin biopsies from each of these patients were sent to Philip E. LeBoit, MD, professor of clinical pathology and dermatology at the University of California, San Francisco. Along with his fellow, Shawn E. Cowper, MD, now assistant professor of dermatology and pathology at Yale University School of Medicine in New Haven, Conn., and other colleagues, he examined these biopsies and observed histologic features similar to one another but that were unique.
