Rheumatology caught the attention of the broader medical community with an article in the Journal of the American Medical Association showing that only 63% of rheumatoid arthritis (RA) patients in Medicare Advantage programs received disease-modifying antirheumatic drugs (DMARDs) from 2005 to 2008.1 Lower than the overall DMARD use rates reported by the National Center for Quality Assurance in 2008, which range from 70% for Medicare plans to 85% for commercial plans, a treatment gap is apparent for RA patients age 65 years and older. Given the average age of diagnosis for RA is 60 years, this age-related gap is disconcerting.
The good news is that the RA treatment gap in older patients is already narrowing. “The fact that 67% of the Medicare patients were on DMARDs in 2008, up from 59% in 2005, is progress,” says Stanley Cohen, MD, clinical professor in the department of internal medicine at the University of Texas Southwestern Medical School in Dallas and past president of the ACR. However, the bad news is that DMARD use rates varied from 16% to 87% across Medicare Advantage plans.
Economics plays a significant factor for healthcare plans and patients. Patients in for-profit Medicare Advantage plans were less likely to get DMARD therapy than those in not-for-profit plans. Lead author of the JAMA study Gabriela Schmajuk, MD, MS, rheumatology instructor at Stanford University in Stanford, Calif., notes this finding is not unique. Studies of quality measures consistently find lower performance rates among for-profit plans compared with not-for-profit plans, even after adjusting for patient characteristics.
Despite the Medicare coverage for prescriptions, a substantial burden of cost still remains with patients. Patients enrolled in Medicare Advantage programs pay 28% of DMARD medication costs. Biologic therapy can cost a patient upwards of $4,000 annually out of pocket with Medicare.2 Not surprisingly, lower income is a barrier to DMARD access. Only 55% of patients with low incomes receive treatment, compared with 64% of patients with higher incomes.
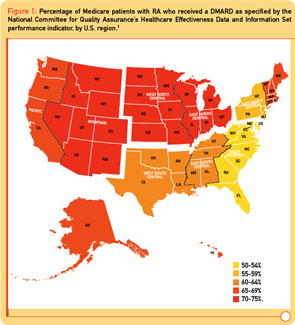
Two surprising additional findings were large geographic variations in DMARD use and a 10%–30% decrease in DMARD use in patients age 75 years and older relative to patients age 65 to 69 years. In the Middle Atlantic and Southeastern states, DMARD use is significantly lower (8%–15%) than the rest of the United States (see Figure 1). Additional factors associated with decreased DMARD use were male sex, black race, and lower socioeconomic status (see Table 1).
Reflecting Real Life in Quality Measures
The large age disparity, with only 13% of RA patients age 85 years and older receiving DMARD therapy, raises the question of what are appropriate target rates for DMARD use among various RA patient populations. Dr. Cohen notes, “In a patient who is 87 years old with mild disease, we clinicians are not worried about progressive disability in 20 years. If they have diabetes, chronic heart disease, or lung disease, we choose not to treat them with a DMARD.”


