The recently released PREDMETH study results indicate that methotrexate can be considered a real alternative to prednisone for patients with pulmonary sarcoidosis.


Deborah Levenson |
The recently released PREDMETH study results indicate that methotrexate can be considered a real alternative to prednisone for patients with pulmonary sarcoidosis.

Jude Al Qaqaa, MD, Vladimir Falb, DO, & Kaitlyn Buzard, DO |
Giant cell arteritis (GCA), is an inflammatory vasculitis that involves large- and mediumsized arteries, most commonly the cranial branches of the carotid artery.1 It is seen in individuals 50 years and older.1 The most typical manifestation is new-onset headache with scalp tenderness and jaw claudication. 2 The most feared complication associated with GCA is permanent…

Bryn Nelson, PhD |
CPPD is notoriously difficult to diagnose due to its diverse presentations & uncertain etiology. Recent advances have helped rheumatologists better understand its risk factors, classify, diagnose & treat the condition.

Vivekanand Tiwari, MD, Emily Campbell, MD, Joshua Skydel, MD, Bryan Savage, MD, Monica Dimambro, Todd MacKenzie, PhD, & William F. Rigby, MD |
Background/Purpose Polymyalgia rheumatica (PMR) treatment is primarily based on long-term corticosteroids, which results in significant toxicities. Studies have shown that patients with PMR are exposed to years of corticosteroid treatment.1,2 In a single academic center cohort, we found that 76% of patients remained on steroids at the end of two years.3 In a second cohort…
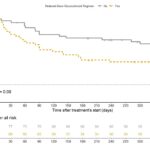
SAN DIEGO—In a study titled Real-Life Use of the PEXIVAS Reduced-dose Glucocorticoid Regimen in Granulomatosis with Polyangiitis and Microscopic Polyangiitis, Nagle et al. evaluated the efficacy and safety of the reduced-dose glucocorticoid regimen in a real-world setting. Background/Purpose Glucocorticoids (GCs) in combination with rituximab (RTX) or cyclophosphamide are the cornerstone of treatment for patients with…

Megan Elizabeth Bowles Clowse, MD, MPH & David Leverenz, MD |
As rheumatologists, we have a love-hate relationship with the corticosteroid prednisone, a feeling many of our patients share. It’s our most effective medication to quickly shut down an overactive immune system. When we have a patient with life- or organ-threatening autoimmune disease—severe lupus affecting the kidneys or vasculitis causing hemorrhage in the lungs, for example—large…
Marcela A. Ferrada, MD, Anjali Takyar, MD, & James D. Katz, MD |
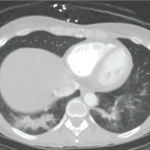
Relapsing polychondritis (RPC) is a systemic and, in some cases, fatal disease. Dyspnea with findings of small airway disease—even in the absence of the more commonly associated tracheobronchial abnormalities or pathognomonic clinical findings, such as saddle nose and cauliflower ear—may be presenting signs and symptoms of relapsing polychondritis. Below, we present a case demonstrating that…
BALTIMORE—Rheumatologists may not think about osteoporosis on a daily basis, but they should, said Dr. Karl Insogna, the Ensign Professor of Medicine at Yale University School of Medicine and director of the Yale Bone Center in New Haven, Conn., in his recent lecture at the Maryland Society for the Rheumatic Diseases. With approximately 75 million…

A recent study found that dermatology patients taking long-term steroids are not always evaluated for steroid-induced osteoporosis…
Treatment with oral methylprednisolone may be associated with an increased risk of serious adverse events, specifically infection, in patients with IgA nephropathy. Despite the five-times higher risk, study results also showed a three-times lower risk of kidney failure for the treatment group…