Clinical Case
RB, a 66-year-old man, presented to the hospital in July 2011 with left-sided visual loss (OS), headache, hematuria, and symptoms of a chronic sinusitis. He was in his usual state of health until the summer of 2009, when he began to develop frequent sinus infections manifesting with headache, sinus pain, and nasal congestion without epistaxis or crusting. He was treated with multiple courses of antibiotics, each time with improvement of his symptoms.
In February 2011, he began to have headaches that did not resolve with antibiotic treatment. Shortly thereafter, he developed urinary frequency, urgency, weak stream, and intermittent gross hematuria. He was seen by a urologist and the diagnosis of benign prostatic hypertrophy was made on the basis of a digital rectal exam and a normal prostate-specific antigen (PSA) level. Several weeks later, he developed incontinence and was diagnosed as having a neurogenic bladder requiring self-catheterization. In March 2011, he was hospitalized at another hospital for severe headache. At that time, computed tomography (CT) imaging of the brain revealed chronic sinusitis with no other abnormalities. A chest X-ray was unremarkable. A sinus biopsy showed nonspecific inflammatory changes and the antineutrophil cytoplasmic antibody (ANCA) testing was normal. He was discharged home to complete a course of antibiotics for the treatment of his sinusitis.
Send us Your Case Suggestion
Have you managed a patient with an unusual rheumatologic problem that you would want to present to a larger audience? Consider submitting your case to The Rheumatologist.
We are looking for interesting cases that are well written and provide useful teaching points to the reader. Send an outline of your case presentation to Simon Helfgott, MD, at [email protected], or visit www.The-Rheumatologist.org for more information.
In April 2011, he developed a urinary tract infection due to Candida albicans. His course was complicated by candidemia, which was treated with a two-week course of fluconazole.
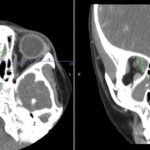
Over the following month his headache persisted and he developed eye pain, diplopia, and numbness in the V1–V2 distribution of the trigeminal nerve. He was admitted to another hospital, where a CT of the brain showed a destructive sinus process that was invading into the left orbital wall. He underwent a second sinus biopsy, which demonstrated acute and chronic inflammation without evidence for vasculitis, granulomas or invasive fungal disease. Sinus tissue cultures grew Staphylococcus aureus and he was started on doxycycline. After one month of therapy he did not note any improvement in his symptoms and began to notice new visual loss in his left eye. He was referred to our hospital.