Treatment with denosumab for patients with RA and glucocorticoid-induced osteoporosis led to greater increases in bone mineral density of the lumbar spine and hips of patients than treatment with risedronate.


Treatment with denosumab for patients with RA and glucocorticoid-induced osteoporosis led to greater increases in bone mineral density of the lumbar spine and hips of patients than treatment with risedronate.
Reuters Staff |
NEW YORK (Reuters Health)—The RANKL inhibitor denosumab is superior to the bisphosphonate risedronate in increasing bone-mineral density (BMD) at the lumbar spine in patients just starting or continuing steroid therapy, according to 12-month results of a 24-month randomized controlled study. “Glucocorticoid-induced osteoporosis is the most common form of secondary osteoporosis and increases the risk of…
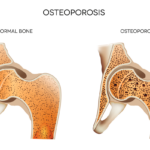
The ACR recently released an update on the prevention and treatment of glucocorticoid-induced osteoporosis.1 The guideline, which includes information on the new therapies abaloparatide and romosozumab, emphasizes the importance of shared decision making by patients and clinicians, and also gives information on the importance of sequential therapy after stopping certain osteoporotic prevention therapies. Fracture Prevention…

A study from Amigues et al. found that bisphosphonate-associated osteonecrosis of the jaw is rare in patients with osteoporosis and may occur more often in patients treated with injectable zoledronic acid than in those treated with the oral bisphosphonates.

Using three complicated patient cases, Kenneth G. Saag, MD, MSc, shared his expertise on osteoporosis and walked through his thought process and the literature, during a session of the 2022 ACR Education Exchange.
Lisa Rapaport |
(Reuters Health)—It takes 12.4 months of bisphosphonate therapy to prevent one nonvertebral fracture per 100 postmenopausal women with osteoporosis, a meta-analysis of randomized clinical trials suggests.1 Researchers examined data on 10 randomized clinical trials with a total of 23,384 women who had an osteoporosis diagnosis based on either existing vertebral fractures or a bone mineral…

Sarah F. Keller, MD, & Marcy B. Bolster, MD |
It is well known that hip fractures are associated with significant morbidity and mortality: Mortality increases 15–25% in the year following a hip fracture.1–5 We know that treating osteoporosis prevents fractures and improves patient survival. But is there a relationship beyond this? Several studies have found that bisphosphonate therapy is associated with a reduction in…

Matthew Phelan |
NEW YORK (Reuters Health)—Long-term glucocorticoid users see greater gains in spine bone-mineral density when treated with the monoclonal antibody denosumab vs. oral alendronate, a small clinical trial shows. The drug also proved superior at lowering bone-turnover markers at 12 months, researchers in Hong Kong report in Bone.1 “Denosumab may be considered as an alternative first-line…

ACR Convergence 2020—At two plenary sessions, speakers highlighted key findings, including results on the QTc interval in patients on hydroxychloroquine, and data from a study on denosumab vs. alendronate for glucocorticoid-induced osteoporosis. The QTc Interval & Hydroxychloroquine The safety profile and optimal dosing of hydroxychloroquine has been a topic for decades because it is known…

In a clinical trial, researchers compared the efficacy of abaloparatide with alendronate in reducing the risk of fracture among postmenopausal women with osteoporosis. The findings suggest initial treatment with abaloparatide may result in greater vertebral fracture reduction than alendronate…