SAN DIEGO—Kawasaki disease (KD) is not going away. These words, spoken by Jane C. Burns, MD, director of the Kawasaki Disease Research Center in the department of pediatrics at the University of California, San Diego, in La Jolla, set the context and tone for a session at the 2013 ACR/ARHP Annual Meeting, held October 26–30. [Editor’s Note: This session was recorded and is available via ACR SessionSelect at www.rheumatology.org.] The session was devoted to providing rheumatologists with tools to recognize and treat KD.
Citing unpublished epidemiological data from Japan, Dr. Burns highlighted that almost 14,000 new cases of KD were diagnosed in 2012 and that one in every 85 children in Japan is predicted to develop KD during the first 10 years of life. In the United States, she said, it is estimated that one in 1,600 adults will have had KD by 2030.
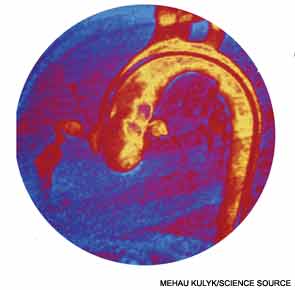
During the session, entitled “Kawasaki Disease: Putting Out the Fire,” a panel of experts provided updated information on the diagnosis and treatment of KD with an emphasis on the need for early detection to minimize complications, including the potential for the formation of coronary artery aneurysms.
Kawasaki Disease: What It Is and What It Is Not
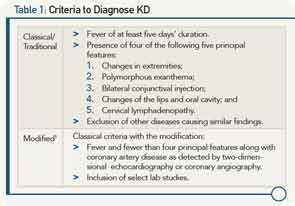
Knowing how to recognize KD and make the differential diagnosis from other diseases is not easy, and requires familiarity with an evolving understanding of what the disease is, according to Robert Sundel, MD, program director in rheumatology at Boston Children’s Hospital, and associate professor of pediatrics at Harvard Medical School in Boston. He emphasized the limitations of the classic or traditional criteria once used to diagnose KD, and discussed more recently developed modified criteria that expanded the differential diagnosis of KD (see Table 1).
Among key features that led to formulation of the modified criteria was the recognition that many patients with KD have concurrent infections, complicating determination of which other conditions to consider in the differential diagnosis. Further, evolving recognition of cardiac involvement in patients who do not meet classical criteria for KD necessitated alternative approaches to optimize outcomes. Occult cardiac involvement in patients with KD includes myocarditis and, importantly, coronary artery aneurysms, he said, emphasizing that the presence of cardiac involvement is a major prognostic determinant with a mortality rate of 1.5% in untreated patients that falls to less than 0.1% in treated patients.