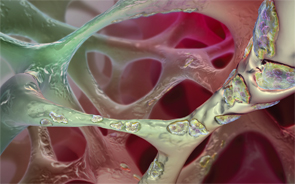
Osteoclast activity is essential in the maintenance, repair and remodeling of bones.
Gary Carlson/sciencesource.com
SAN FRANCISCO—Post-menopausal women with osteoporosis, previously treated with oral bisphosphonates, had greater increases in bone density when taking denosumab compared with zoledronic acid over a year’s time, according to a study presented at the 2015 ACR/ARHP Annual Meeting.
The findings were discussed in the Discovery 2015 plenary session, which focused on new research. In the session, researchers also discussed genetic mutations linked with early-onset auto-inflammatory disease and new findings on the TH17 T cell response in systemic sclerosis.
In the Bones
In the denosumab (DMAb) study, researchers set out to examine the effectiveness of two alternatives to oral bisphosphonates for osteoporosis.1 Oral bisphosphonates are the most commonly used treatment for the disease, but adherence can be low, and not all patients respond well.
Less frequently dosed bisphosphonates—such as once-a-year zoledronic acid (ZOL)—are an option for patients who are intolerant to or have failed oral bisphosphonates. Patients can move from one bisphosphonate to another, but the benefits of that approach haven’t been shown, said Paul Miller, MD, medical director of the Colorado Center for Bone Research, who presented the findings.
The study included post-menopausal women at least 55 years old who had been on oral bisphosphonates for at least two years, with a bone mineral density T-score of -2.5 or worse and C-terminal telopeptide (CTX) levels, a marker of bone breakdown, of no higher than 500 pg/mL.

Dr. Miller
The patients were randomized to the two groups, with 321 in the DMAb group, who were given 60 mg subcutaneously every six months, and 322 in the ZOL group, who were given a once-yearly IV dose of 5 mg of zoledronic acid.
The groups were balanced in terms of age, years since menopause and bone densities.
After 12 months, lumbar spine bone density—the primary endpoint—had increased by 2.1% more in the DMAb group, or more than double what was seen in the ZOL group (P<0.0001). Significantly greater increases were also seen in bone densities for total hip, femoral neck and 1/3 radius.
Levels of CTX and P1NP, another marker of bone breakdown, rose gradually among those on ZOL, but remained relatively constant among those taking DMAb, Dr. Miller showed.
The number of serious adverse events was similar for the two groups.
“In post-menopausal women with osteoporosis who had received prior oral bisphosphonates for at least two years or more, transitioning to denosumab resulted in significantly greater increases in bone density compared with zoledronic acid at all measured skeletal sites,” Dr. Miller said.
It’s the latest study to show the superiority of denosumab in patients who’ve previously been treated with bisphosphonates. Previous studies have compared the drug to risedronate, alendronate and ibandronate.1-4
“This study completes a suite of trials,” he said, “that shows transitioning from a bisphosphonate to DMAb provides greater increases in BMD (bone mineral density) and reduction in bone turnover markers compared to maintaining therapy with another bisphosphonate.”
A20 Mutations
Dr. Zhou
In another study, Qing Zhou, PhD, a researcher with the National Human Genome Research Institute of the National Institutes of Health, described a new auto-inflammatory disease involving mutations in the TNFAIP3 gene, which causes haploinsufficiency of the A20 anti-inflammatory protein.5
“The patient presents with a childhood onset of systemic inflammation and some features resemble Behçet’s disease,” Dr. Zhou said. The features include skin lesions, oral and genital ulcers, ocular inflammation, arthralgia and arthritis and GI inflammation. Researchers have called the disease HA20.
The work began with two families in whom A20 mutations were found with exome sequencing, which led to the screening of 150 other patients with similar clinical features.
Those with the A20 mutations, researchers found, do not inhibit tumor necrosis factor-induced activation of the NF-kB inflammatory pathway. And there is an overproduction of inflammatory cytokines—such as IL-1-beta, tumor necrosis factor and IL-6—in these patients, they found.
These A20 mutations activate the NLRP3 inflammasome, which has been recognized as the body’s most influential and versatile signaling platform for inflammatory disorders.6
There have been positive, though early, results using an agent targeting IL-1-beta, Dr. Zhou said.
“These findings raise the possibility of new targeted therapies for this spectrum of disease,” she said.
Opportunity for Scleroderma Treatment
In other findings, Raymond Ong Jr., a researcher at Singapore General Hospital, described new insights into the interplay between the microenvironment of the skin and the periphery in scleroderma that might provide an opportunity for treatment.

Mr. Ong
In scleroderma (SSc), he said, there is an unmet need to identify and describe immune cell phenotypes that are involved in scleroderma pathogenesis to drive development of targeted therapies.
In this trial, he said, researchers hypothesized that immune signatures found at the interface of the microenvironment and systemic immunity both define disease pathogenesis and dictate outcomes in scleroderma patients.
Researchers employed an array of “high throughput” technologies to study 23 subjects—including scleroderma subjects and healthy controls—in search of immune signatures clustered meaningfully at the level of single cells. They used gene expression studies with human dermal fibroblasts stimulated with an autoantigen (Topo I) that’s linked with SSc; mass spectrometry analysis of peripheral blood; and RNA sequence analysis.
Researchers found an increased frequency of pro-inflammatory TH17 phenotype in scleroderma subjects compared with healthy controls.
They also showed, for the first time, that skin-derived IL-11 cytokine appears to be a requirement for the generation of the TH17 T cell response.
“There is a functional interplay,” Mr. Ong said, “between the microenvironment and the periphery in generating a pro-inflammatory TH17 response in scleroderma.”
Thomas R. Collins is a medical writer based in Florida.
Second Chance
If you missed this session, it’s not too late. Catch it on SessionSelect.
References
- Miller PD, Pannacciulli N, Brown JP, et al. A randomized double-blind study of denosumab compared with zoledronic acid in postmenopausal women with osteoporosis previously treated with oral bisphosphonate. Presented at the 2015 ACR/ARHP Annual Meeting. Nov. 7–11, 2015. Abstract 898.
- Roux, C, Hofbauer, LC, Ho PR, et al. Denosumab compared with risedronate in postmenopausal women suboptimally adherent to alendronate therapy: Efficacy and safety results from a randomized open-label study. Bone. 2014 Jan;58:48–54.
- Recknor C, Czerwinski E, Bone HG, et al. Denosumab compared with ibandronate in postmenopausal women previously treated with bisphosphonate therapy: A randomized open-label trial. Obstet Gynecol. 2013 Jun;121(6):1291–1299.
- Kendler DL, Roux C, Benhamou CL, et al. Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res. 2010 Jan;25(1):72–81.
- Zhou Q, Wang H, Schwartz D, et al. HA20: A novel autoinflammatory disease caused by haploinsufficiency of A20, encoded by TNFAIP3. Presented at the 2015 ACR/ARHP Annual Meeting. Nov. 7–11, 2015. Abstract 899.
- Vande Walle L, Van Opdenbosch N, Jacques P, et al. Negative regulation of the NLRP3 inflammasome by A20 protects against arthritis. Nature. 2014 Aug 7;512(7512):69–73.


