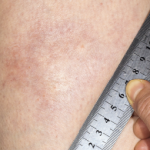
Figure 3. The skin of the patient’s lower extremities was shiny, thickened and hairless.
The labs at the time were significant for an albumin of 2.1 gm/dL, a thyroid-stimulating hormone of 1.92 mIU/mL, a 24-hour urine protein of <0.14 gm/24h, a faint IgG kappa restriction (kappa free light chains 3.45 mg/dL with kappa lambda free light chain ratio 1.96), and a white blood cell count of 7.9 x 103 mcL with 21.9% eosinophils. An endoscopy and a colonoscopy were unremarkable; biopsies showed non-specific duodenitis and gastritis. Bone marrow biopsy was normal. Ultimately, she was referred to rheumatology for further workup.
On presentation at the rheumatology clinic, she complained of new symptoms, including jaw locking, hair loss (including loss of her pubic hair), hand swelling, 40 minutes of morning stiffness, fevers, chills and stocking distribution paresthesias.