
Low back pain is a symptom associated with about 60 different problems that range from muscle strains to spondyloarthritis to osteomyelitis. In a presentation at the 2013 ACR State-of-the-Art Clinical Symposium, held April 20–21 in Chicago, David Borenstein, MD, said that low back pain is challenging for physicians, given the multiple therapies available, the differences between acute and chronic pain, the conflicting research about the effectiveness of the therapies, and the time often required to find an adequate solution for chronic pain.
“Most of us don’t believe that we take care of pain and think that we only take care of the immune system. But, in fact, we do take care of pain, and it is an important part of our job as rheumatologists,” he said. There is little consensus among experts about the definition of low back pain, the differences between chronic and acute low back pain, or how research studies should be designed, said Dr. Borenstein, clinical professor of medicine at the George Washington University Medical Center in Washington, D.C. There is consensus, however, that no single therapy is adequate to treat all chronic pain.
In describing therapy for an average patient with chronic low back pain, Dr. Borenstein said he would treat the patient with several nonpharmacologic therapies, including exercise with range of motion and walking on a treadmill. Patients who smoke are encouraged to stop, and those not sleeping well are advised to cut back on their caffeine consumption. A change in job responsibilities may help patients reduce stress. Over the course of therapy, Dr. Borenstein said that he might prescribe a nonsteroidal antiinflammatory drug (NSAID), an opioid, an antidepressant to increase serotonin production, a topical agent, or a muscle relaxant.
“We need to use multiple categories of therapy at lower doses to maximize the effect and limit the toxicity. Chronic is, in fact, for a long time and there will be ups and downs, but as their physician, you need to keep trying.”
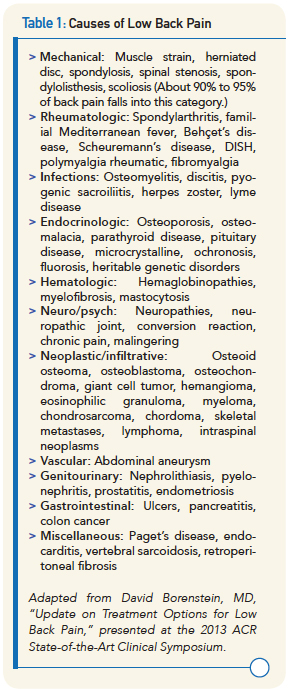
Dr. Borenstein said he classifies low back pain into several groups that represent the causes of the pain (see Table 1). “This is a way of taking those 60 different illnesses and trying to approach them in a thoughtful manner both diagnostically and therapeutically to deal with these various types of medical problems that come into your office.”
Epidural Injections
Dr. Borenstein highlighted recent research examining the efficacy of epidural injections for sciatic pain. One study compared pain relief provided by injections of steroids, saline, or etanercept in 84 adults.1 Steroid therapy gave greater reduction in pain, with 75% of patients in that group reporting 50% or better pain relief at one month, compared with 50% of patients in the saline group and 42% in the etanercept group. “This suggests that modest short-term pain relief is possible with epidurals,” Dr. Borenstein said.
