The 2024 Image Competition showcased images representing a diverse range of pediatric patients. Here, we showcase the images from Europe and Central Asia, which were selected by ACR Convergence 2024 attendees in the first plenary session to receive the People’s Choice Award.
A Rare Presentation of a Rare Disease
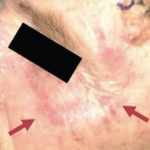
An 18-month-old boy from Angola was brought to the hospital with a one-year history of neurodevelopmental regression—notably in his gait—as well as proximal myopathy (image B), scattered skin ulcers (images C, E, F), Gottron’s papules (image D), oral ulcers and prolonged fever. He had no significant family history.
Laboratory tests revealed microcytic anemia (i.e., hemoglobin 7.5 g/dL) and thrombocytosis, with normal creatine kinase and aldolase. Aspartate aminotransferase and lactate dehydrogenase were elevated. Inflammatory markers included an erythrocyte sedimentation rate of 43 mm/h, C-reactive protein at 6.7 mg/dL and ferritin at 1,633 ng/mL.
Serologic testing helped rule out HIV, Epstein-Barr virus, cytomegalovirus, toxoplasmosis, rubella, syphilis, hepatitis B and hepatitis C. Mycobacterium tuberculosis was not identified on skin biopsy, in gastric juices or in blood via polymerase chain reaction.
Autoimmune testing revealed anti-NXP2 antibodies, but other tests yielded no significant findings. Anti-nuclear antibody titers were 1:80. A muscle biopsy confirmed the diagnosis of juvenile dermatomyositis.
Since the diagnosis, the patient has undergone treatment with pulse-dose and maintenance corticosteroid therapy, human immunoglobulin, cyclosporine, methotrexate and mycophenolate mofetil. Complications included arterial hypertension (managed with two anti-hypertensive agents); secondary infection of skin ulcers caused by Pseudomonas aeruginosa, Escherichia coli and Staphylococcus aureus (treated with antibiotic therapy); and acute gastroenteritis due to Cryptosporidium (treated with anti-parasitic medication).
The patient is under multidisciplinary care, with clinicians specializing in rheumatology, dermatology and rehabilitation. Clinical improvement has been slow, with worsening of skin lesions observed during corticosteroid tapering.
Learn More
Screening for myositis-specific antibodies can help clinicians identify and predict specific manifestations of myositis. A muscle biopsy can provide further evidence to confirm or rule out a diagnosis of juvenile dermatomyositis.
To learn about potential treatment options for dermatomyositis, read our article, “Type I IFNs in Cutaneous Lupus & Dermatomyositis.”
Ana Rita Fradique, MD, is a member of the pediatric rheumatology team at the Hospital Pediátrico de Coimbra, Coimbra Local Health Unit (ULS Coimbra), Coimbra, Portugal.
About the Contest
Images from the ACR’s annual contest are added to the Rheumatology Image Library Look for all the winning images in future issues and on our website.