 The ACR recently released an update on the prevention and treatment of glucocorticoid-induced osteoporosis.1 The guideline, which includes information on the new therapies abaloparatide and romosozumab, emphasizes the importance of shared decision making by patients and clinicians, and also gives information on the importance of sequential therapy after stopping certain osteoporotic prevention therapies.
The ACR recently released an update on the prevention and treatment of glucocorticoid-induced osteoporosis.1 The guideline, which includes information on the new therapies abaloparatide and romosozumab, emphasizes the importance of shared decision making by patients and clinicians, and also gives information on the importance of sequential therapy after stopping certain osteoporotic prevention therapies.
Fracture Prevention
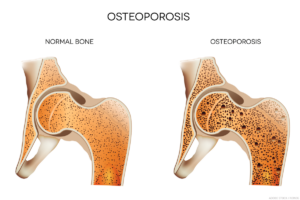
Despite efforts to reduce or eliminate glucocorticoid therapy, many patients with rheumatic or other diseases require treatment over the long term. Yet glucocorticoids increase the risk of bone fractures, especially vertebral fractures, with patients taking higher doses of glucocorticoids and/or longer duration of therapy carrying the greatest fracture risk.
Mary Beth Humphrey, MD, PhD, co-principal investigator of the guideline, professor of medicine and chief of the Rheumatology, Immunology and Allergy Section, the University of Oklahoma Health Sciences Center, Oklahoma City, notes that common fractures, such as those of the wrist or hip, can prevent patients from performing their regular activities of daily living, and mortality rates after a hip fracture may approach 25% in the following year.2
The other co-principal investigator of the guideline is Linda Russell, MD, director of the Osteoporosis and Metabolic Bone Health Center for the Hospital for Special Surgery, New York City. She notes that, for many years after the discovery of corticosteroids, no medical society took ownership of glucocorticoid-induced osteoporosis. But in 1996, the ACR released its first clinical guideline to help rheumatologists and physicians in other specialties manage glucocorticoid-induced osteoporosis.3 The ACR updated these guidelines several times, most recently in 2017.4
Like other recent ACR guidelines, these employ the GRADE methodology (i.e., Grading of Recommendations, Assessment, Development and Evaluation). After considering a comprehensive review of the medical literature on this topic, a voting panel made strong or conditional recommendations on specific management questions based on the PICO framework (i.e., Patient/Intervention/Comparator/Outcomes).
The following is a discussion of some of the key areas of interest addressed in the new glucocorticoid-induced osteoporosis guideline. For more detail and context, and for information about additional key topics, such as osteoporotic treatment in special populations (e.g., children, patients with kidney transplant, people who may become pregnant and patients receiving very high-dose glucocorticoids), refer to the full guideline.1
Prevention Approaches
Multiple agents are now available for the treatment of osteoporosis and, specifically, for glucocorticoid-induced osteoporosis. The first agents specifically developed for osteoporosis were bisphosphonates, approved by the U.S. Food & Drug Administration (FDA) in 1995. These anti-resorptive agents are available in multiple formulations, including in combination with vitamin D and as intravenous (IV) injections, although these carry a slightly higher risk profile than oral formulations.5

