Monosodium urate (MSU) crystal deposition commonly occurs within the distal appendicular skeleton. The peripheral nature of gout is a hallmark feature described in the ACR and the European League Against Rheumatism (EULAR) clinical practice guidelines.1
In this article, we report a rare presentation of a common disease: a case of axial gouty arthropathy masquerading as infectious discitis.
The Case
Our patient is a 66-year-old man with longstanding, untreated hyperuricemia, chronic kidney disease and poorly controlled diabetes abruptly transitioned from colchicine to allopurinol due to the cost of colchicine. Approximately 72 hours after the switch, he presented at a local emergency department with fever, confusion and severe low back pain.
Unenhanced magnetic resonance imaging of his lumbar spine revealed diffuse T2 hyperintensity, concerning for L4–L5 discitis. His clinical presentation confusion, fever, atrial fibrillation with rapid ventricular response and tachypnea—and laboratory evidence of leukopenia and elevated inflammatory markers were concerning for sepsis from a spinal source. He was treated in accordance with the institutional sepsis bundle and transferred to our tertiary care center.
Biopsy of the suspicious lesion within the L4–L5 intervertebral disc space showed purulent material without organism; however, the pathologist noted abundant monosodium urate (MSU) crystals. Blood cultures prior to antibiotics and subsequent disc cultures were negative. A definitive diagnosis of acute axial gout was established. Consultation with a rheumatologist confirmed a polyarticular peripheral gouty attack in the left shoulder, elbow and wrist.
Due to this patient’s heavy disease burden and difficult-to-control hyperglycemia with intravenous glucocorticoids, he was initially treated with three intravenous doses of anakinra and slowly tapered to a maintenance dose of methylprednisolone with colchicine while titrating allopurinol to achieve a uric acid goal of less than 5.0 mg/dL.
Our patient silently suffered from chronic hyperuricemia, which resulted in a heavy disease burden. MSU deposits formed tophi within the intervertebral disc of the lumbar spine.

This MRI of the spine shows inflammatory involvement of the L4 and L5 disc space.

Periarticular end plate edema is apparent at the L4–L5 facet joints.
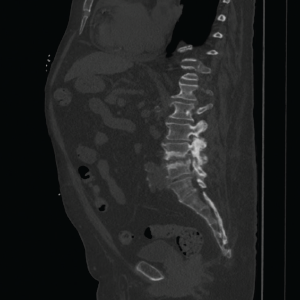
Advanced multi-level degenerative changes, as well as end plate sclerosis and erosions, are shown. They are the worst at the L4–L5 intervertebral
disc space.
Discussion
Gout is characterized by the ACR/EULAR as “at least one episode of swelling, pain or tenderness in a peripheral joint or bursa.”2 Note the word peripheral. It is commonly felt that axial involvement is rare.3 Only 133 cases of spinal gout were reported from 1950–2015.4 Many suspect this phenomenon is more prevalent than commonly appreciated due to its under-reported nature.5
The gold standard for diagnosis of gouty arthropathy is microscopic evidence of MSU crystals from the joint aspirate. Dual-energy computer tomography (DECT) is helpful in cases in which the diagnosis through biopsy is inconclusive due to the small concentration of MSU crystals usually seen early on in the disease.6 During the acute phase of the disease, joint aspirations may not demonstrate MSU crystals 25% of the time.7 Joint space inaccessibility or aspiration contraindications may make a noninvasive modality the preferred choice for an examination.6,8
DECT offers the advantage of estimating the urate crystal volume load, which helps in monitoring the treatment outcome.9 It also helps differentiate between other forms of crystalline arthropathy.6 Ultrasound imaging can detect urate crystal deposits within cartilage and within the joint fluid, described as the double contour sign and starry sky, respectively.10 DECT and ultrasound have similar sensitivity for detecting gouty arthritis; however, the rate of false-negative cases was higher with DECT.10
Our patient did not undergo a DECT due to lack of availability, but had ultrasound-guided peripheral joint aspiration. A computed tomography of the spine showed facet involvement with end plate erosions, surrounded by sclerosis and calcifications. The sclerosis indicates a more chronic process, and the facet joints are typically not affected in infectious discitis or osteomyelitis. These radiological findings, along with negative blood cultures, MSU crystals in aspirate, peripheral joint involvement and poor response to antibiotics, helped differentiate spinal gout from infectious discitis.
