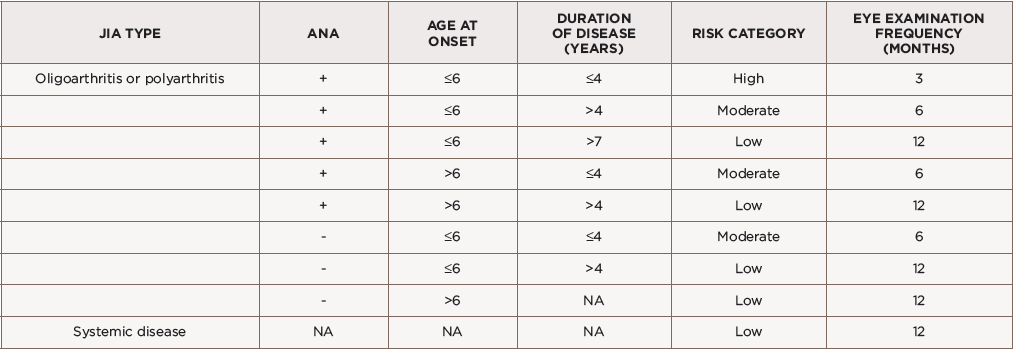
(click for larger image) Table 1: American Academy of Pediatrics Screening Guidelines for Children with JIA*
ANA = anti-nuclear antibodies; NA = not applicable
*Adapted from Cassidy et al., 2006.
On the other end of the spectrum, children with systemic or polyarticular rheumatoid factor (RF) positive JIA are considered at low risk, with less than 1% developing uveitis, and these patients can be screened every 12 months.20,21 Additional factors such as female sex, Caucasian race and non-Hispanic ethnicity have been associated with uveitis susceptibility and ocular complications, but these factors are not currently used in the screening guidelines.
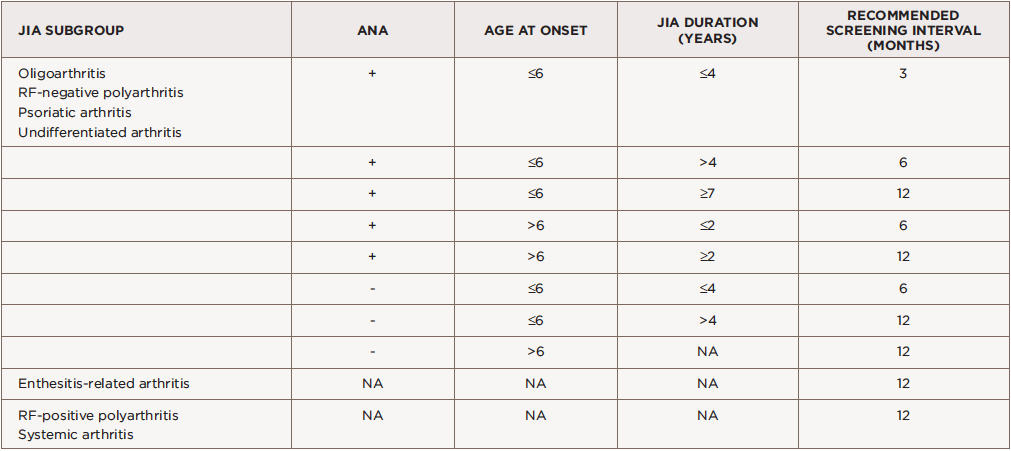
(click for larger image) Table 2: Screening Recommendations in JIA Classified by International League of Associations for Rheumatology (ILAR) Criteria*
ANA = anti-nuclear antibodies; RF = rheumatoid factor; NA = not applicable
*Adapted from Heiligenhaus et al., 2007.
Once uveitis is diagnosed, the frequency of eye examinations is not standardized; it’s based on the patient’s response to therapy and ocular complications.20
Risk Factors

The slit lamp examination should include measurement of cell and flare by the Standardization of Uveitis Nomenclature (SUN) and careful documentation of any complications of uveitis.
As with other autoimmune diseases, the etiology of uveitis is likely multifactorial. Children with HLA-DRB1 alleles have increased risk for uveitis.24-29 Studies have also investigated potential biomarkers in JIA-U, including erythrocyte sedimentation rate (ESR), interleukin 29/interferon λ1 (IL29/IFNλ1), transthyretin (TTR) and other cytokines and chemokines.30-34 Identifying biomarkers that aid in screening, monitoring disease and treatment decisions may help improve outcomes in uveitis. Active research is underway to identify biomarkers in tears and aqueous humor associated with uveitis susceptibility, treatment response and ocular outcomes.
Various risk factors have been associated with ocular complications and visual impairment, including race, sex, ANA positivity and uveitis age and onset. African-American children have lower risk of JIA-U compared with non-Hispanic whites. However, if diagnosed, African Americans may be at higher risk for ocular complications and vision loss.35,36 Also, Hispanic ethnicity is associated with a higher rate of vision loss at baseline.5 Although females have an increased likelihood of uveitis, males may be more likely to have severe uveitis at diagnosis.22,37
ANA positivity has been associated with uveitis, but ANA-negative children may have increased complications.38 A short duration between the development of arthritis and subsequent diagnosis of uveitis, and a uveitis diagnosis at a young age, increase risk for severe ocular manifestations.12,22 Children who develop uveitis prior to arthritis diagnosis have increased rates of complications.38-40 This may be due to the asymptomatic presentation of uveitis associated with JIA leading to a delayed diagnosis.
Collaboration with Ophthalmology
Pediatric uveitis management is challenging. Emphasize the importance of regular ophthalmology screening to families, given the asymptomatic nature of uveitis and risk for poor visual outcomes. The eye examination typically consists of measuring monocular best-corrected visual acuity (BCVA), intraocular pressure (IOP), alignment and motility, anterior segment examination by slit lamp exam (prior to the instillation of any eye drops), and pupillary reaction (see Table 3). The slit lamp examination should include measurement of cell and flare by the Standardization of Uveitis Nomenclature (SUN), and careful documentation of any complications of uveitis.41


