During the ophthalmology visit, the patient should be dilated for at least 30 minutes with cyclopentolate 1% and phenylephrine 2.5% drops for a detailed examination of the retina and measurement of refractive error. Measurement of refractive error when the pupils are dilated is essential in all children, especially those with reduced visual acuity, to determine whether vision changes are related to refractive error or amblyopia.
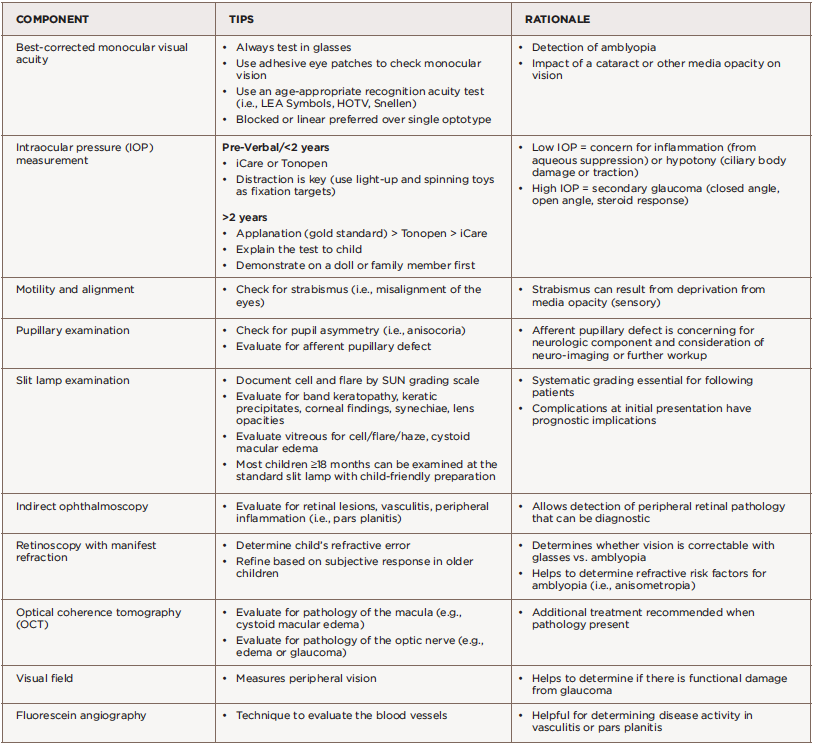
Amblyopia is decreased vision in one or both eyes due to abnormal visual stimulation of the brain in infancy or early childhood. Uveitis can cause amblyopia via changes in refractive error from lenticular changes, glaucoma or deprivation secondary to media opacities such as band keratopathy, cataract, vitreous opacities and cystoid macular edema. Ancillary testing by visual field test (to measure peripheral vision), optical coherence tomography (to measure the thickness of the optic nerve and macula), and fundus photography may be performed based on clinical examination findings. This testing can help monitor complications of uveitis, such as glaucoma or cystoid macular edema.
Close collaboration between the rheumatologist and ophthalmologist is essential to optimize outcomes for the patient. The ophthalmologist closely monitors ocular inflammation through slit lamp exam and manages topical and peri/intraocular ophthalmic medications. The rheumatologist diagnoses and manages associated systemic diseases and treatment with systemic immunosuppressive medications.42 Regular communication is also important in establishing an overall treatment plan for each patient.
Unfortunately, when these evaluations are performed through specialists practicing in different healthcare systems, formal reports may not always be communicated between providers, creating fragmented care and potentially delayed diagnosis and treatment. Combined ophthalmology-rheumatology clinics can address these concerns. A review over a three-year period from a combined pediatric ophthalmology and rheumatology clinic in Edinburgh, Scotland, suggested improved eye screening rates, improved convenience for both patients and providers, and prevention of delayed diagnosis and treatment in patients with uveitis present at their first eye exam.43
Our experience from the combined uveitis clinics at the Cincinnati Children’s Hospital Medical Center in Ohio has shown the advantages of subspecialty collaboration. Our clinic is staffed by both a pediatric ophthalmologist and a pediatric rheumatologist who perform evaluations simultaneously, which leads to a unified approach to care. The ophthalmologist performs an extensive eye assessment to determine the presence and extent of inflammation, and the rheumatologist conducts a full physical exam to evaluate for associated systemic conditions. The specialists can learn from one another, make treatment decisions based on their combined assessment and educate patient and families in real time if systemic therapies are required.