Because of concern for IgG4-related disease, the lung biopsy tissue was retrospectively stained for IgG4+ plasma cells. Referral to the MGH Division of Rheumatology was made. The IgG4+ cell count was 21/hpf with 43% IgG4/IgG ratio. All available pathologic material, including specimens from the pancreas, liver, lung and bone marrow, was reviewed by Vikram Deshpande, MD.
The lung biopsy showed CD68-positive, S-100-negative, CD1a-negative foamy histiocytes not previously appreciated. All were consistent with a diagnosis of ECD.
A clinical decision was made to start 8 mg/kg tocilizumab intravenously every four weeks; prednisone was tapered from 20 mg to 10 mg daily over a three-month period. A repeat PET-CT showed lungs with markedly less uptake and stable fludeoxyglucose avidity in the pancreas and bone (see Figure 2D). Repeat CT scans showed vast improvement in inflammation intra-abdominally and complete resolution of pulmonary ground-glass opacities (see Figure 4A).

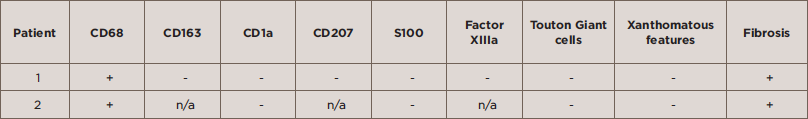
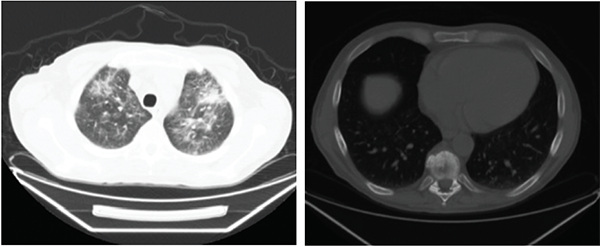
Figures 1C (left) & D (right): Patient 2
Figures 1A–D show the computed tomography (CT) on Patients 1 and 2. 1A is a CT scan of Patient 1 without contrast showing pulmonary ground-glass opacities. 1B is a CT scan of Patient 1 showing a sclerotic lesion at T10. 1C is a CT scan of Patient 2 with contrast showing soft-tissue rind around the kidneys, also seen in Patient 1. 1D is a CT scan of Patient 2 with contrast showing soft-tissue infiltration around the abdominal aorta.
The patient has been in remission without repeat hospitalizations for five years.
Patient 2: A 54-year-old man presented in 2014 to his physician with back and flank pain, low-grade fever and a 7 kg weight loss. Medical history included resolved depression treated with antidepressants, no prior surgeries and no allergies. His family history was unremarkable. He was a married veterinarian with two children and a non-smoker with occasional alcohol use.
On review of systems, he had low-grade fevers, back pain, flank pain and pain in the rhomboid area. He had no neurological complaints, vision symptoms, swollen lymph nodes or cardiopulmonary symptoms. He denied urinary hesitancy or other voiding symptoms. There were no rashes.
Vital signs were normal. Positive findings included lacrimal gland enlargement, goiter (left greater than right side) and several enlarged lymph nodes (up to 2 cm in his axilla and 1.5 cm in the inguinal area). His abdomen was mildly distended, nontender, with no organomegaly. There was no costovertebral angle tenderness. There were hyperpigmented plaques on his distal extremities. Laboratory studies revealed an increased creatinine level, and an ultrasound demonstrated bilateral hydronephrosis. Bloodwork in September 2015 showed WBC 10.7 x 109/L, Hct 35%, platelets 348 x 109 (normal <350), creatinine 98 μmol/L, total protein 60 g/L, albumin 33 g/L, ALP 164 U/L, AST 35 U/L, ALT 74 U/L and high-sensitivity C-reactive protein (HS-CRP) 105 mg/L (normal <5). A lipid panel was normal. He was hepatitis B immune. Urinalysis showed no protein, trace hemoglobin, 11–30 WBCs per HPF, 1–3 RBCs per HPF and a few epithelial cells. The patient’s IgG subclasses were normal.