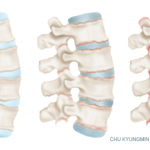
Ankylosing spondylitis primarily affects the joints and ligaments of the spine, but may also have an impact on other joints. Patients experience pain and stiffness that limit mobility in the back and other affected joints. Symptoms can come and go, last for long periods of time and be severe. Anti-tumor necrosis factor (anti-TNF) drugs are prescribed to patients to reduce inflammation in the joints with the hope that they will also prevent joint damage. Although anti-TNF drugs improve symptoms of inflammation, they make patients more vulnerable to infection, leading physicians to wonder if the benefits offset the risks.
In a recent Cochrane review, researcher Lara J. Maxwell, managing editor, Cochrane Musculoskeletal Group at the Ottawa Hospital Research Institute in Canada, and colleagues, report moderate- to high-quality evidence that anti-TNF agents are effective at improving clinical symptoms in patients with ankylosing spondylitis.1
The team analyzed results from randomized controlled trials on the effects of four anti-TNF drugs on ankylosing spondylitis—adalimumab, etanercept, golimumab and infliximab—and concluded there is no evidence of an increase in serious adverse events in patients receiving anti-TNF.
The team identified 21 trials with 3,308 participants published through June 2014. Most of the studies were funded by pharmaceutical companies. The package inserts for anti-TNF agents describe the possible side effects of serious infections, such as tuberculosis or upper respiratory tract infection. Certain types of cancer are also listed as a potential rare complication. The Cochrane review did not find any of these serious adverse events in any of the studies. The authors noted, however, that anti-TNF trials were of short duration (< 24 weeks), and thus enabled them only to draw conclusions about the short-term toxicity profile of anti-TNF. Based on their systemic literature review, they determined that short-term toxicity profile to be acceptable.
Treatment with anti-TNF drugs was associated with improved pain function and slight improvement in spinal inflammation as measured by magnetic resonance imaging. The authors calculated the 40% response according to the improvement criteria of the Assessment of SpondyloArthritis international Society (ASAS40) for each of the different anti-TNF drugs. On average, 13% of patients in the placebo group experienced improvement. By comparison, 46% of patients receiving adalimumab, 43% of patients receiving etanercept, 38% of patients receiving golimimab and 53% of patients receiving infliximab met ASAS40 treatment goals.
Patients receiving anti-TNF treatment also were more likely to achieve partial remission of symptoms when compared with placebo. Partial remission was defined as a value of < 2 on a 0–10 scale of pain, function or inflammation. Placement on the scale was determined by morning stiffness and patient overall well-being. The review found that, although only 3% of patients in the placebo group experienced partial remission, many patients in the treatment groups achieved remission: 19% who received adalimumab, 13% who received etanercept, 16% who received golimumab and 47% who received infliximab.