Patients who smoke, are obese (BMI >35), or carry a diagnosis of inflammatory arthritis are not good candidates for cartilage repair surgery.20 Advanced degenerative changes with more than 50% joint space narrowing are considered a contraindication to cartilage repair in all but the very young who have intolerable symptoms and no other reasonable therapeutic options.
Treatment Algorithm
Once a decision has been made to proceed with cartilage repair, a surgical plan is formulated that defines not only the specific repair technique best suited to address the specific cartilage defect, but also incorporates any procedures required to remedy potential articular comorbidities. Treatment strategies for cartilage repair are based primarily on defect location and size. The two most common locations for cartilage defects are on the (medial) femoral condyle and in the patellofemoral compartment, each with their own treatment algorithms.1,21,22
Tibiofemoral Compartment
The choice of cartilage repair procedure for femoral defects is primarily dictated by defect size. Generally, the less invasive procedures of microfracture and osteochondral autograft transfer (OAT) have demonstrated acceptable outcomes only in defects smaller than approximately 3–4 cm2. Larger defects demonstrated only transient improvement in function, or increased donor site morbidity, respectively.23-26 Both microfracture and OAT consistently produce good and excellent results in 60% to 80% of patients with small lesions (<2–4 cm2) on the femoral condyles.27-30
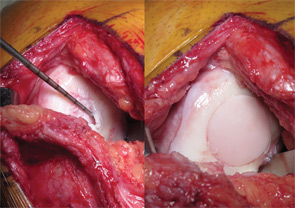
Larger defects therefore are mostly treated with more invasive procedures such as osteochondral allograft transplantation or autologous chondrocyte implantation (ACI). While no studies have been performed to directly compare these more invasive procedures, large cohort studies have demonstrated good and excellent results in more than 70% of patients for each.3,31-35 Generally, defects limited to the articular surface are best treated with ACI, while defects with associated abnormalities of the subchondral bone should be considered for osteochondral allograft transplantation, which replaces both cartilage and the underlying bone.
Patellofemoral Compartment
The patellofemoral (PF) compartment is a difficult location for cartilage repair, and all techniques do worse here compared with the tibiofemoral compartment, due to its more complex geometry and higher shear forces. The importance of correcting adverse factors, such as patellar maltracking, is particularly important in this location.
While microfracture, OAT, and osteochondral allograft have generally good outcomes in the femoral condyles, there is a growing consensus that they should be used cautiously in the patellofemoral compartment except in very specific cases.
Surgical Procedures to Treat Cartilage Defects
Debridement and chondroplasty (removal of degenerated tissue and creation of mechanically stable cartilage with vertical shoulders) is generally performed arthroscopically. This can be the definitive treatment for incidentally found lesions, or initial treatment for symptomatic defects prior to consideration of more invasive cartilage repair procedures. Patients recover quickly after a debridement and chondroplasty, and patients can be fully weight bearing, but should allow pain and swelling to resolve prior to returning to activities.


