NEW YORK (Reuters Health)—Serum biomarkers can discriminate between Crohn’s disease (CD) and ulcerative colitis (UC), according to Danish and Dutch researchers.
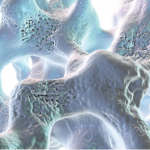
“The biomarker assays measure neo-epitopes, which are fragments of extracellular matrix protein degradation,” Joachim Høg Mortensen, a PhD student at Nordic Bioscience in Herlev, Denmark, told Reuters Health by email.
“These neo-epitopes are increasingly released into the circulation as part of the inflammatory condition, and hence are a direct measure of tissue health and deterioration. This is the core of our sensitive and novel technology,” he explained.
Mortensen and colleagues note that they tested a variety of biomarkers in 72 subjects with CD, 60 with UC and 32 controls without inflammatory bowel disease (IBD). They went on to validate their findings in a further 46 patients with CD and 15 with UC.
Their findings appeared online July 18 in the Journal of Crohn’s and Colitis.
Using the citrullinated and MMP-degraded vimentin biomarker (VICM) and MMP-9-degraded collagen type III (C3M) yielded the best results in differentiating CD and UC. Other markers that helped differentiate CD from UC and UC from non-IBD included type I pro-collagen (P1NP) and C1M.
“The diagnostic sensitivity and specificity for differentiating Crohn’s from colitis were 89% and 83%, respectively, with a diagnostic accuracy of 84%,” Mortensen said.
“The diagnosis of IBD is often difficult and time consuming, and is based on invasive and risk-associated diagnostic procedures including endoscopies, biopsies, and costly MRIs,” he added. “Blood-based biomarkers are objective and non-invasive tools, which potentially could save the clinician’s time and the patient from uncomfortable procedures. Our results indicated that applying this novel technology may aid clinicians in providing the correct diagnosis.”
“Furthermore,” he concluded, “the biomarkers may also be used for assessing burden of the disease, disease prognosis and even monitoring response to treatment.”
Commenting on the findings by email, Dr. Tim de Meij of VU University Medical Centre, Amsterdam, told Reuters Health, “Endoscopy is currently a necessary, invasive tool in the diagnostic process of IBD, which carries a high burden on patients. The search for non-invasive diagnostic biomarkers remains therefore warranted.”
“Here, the authors described the neo-epitopes VICM and C3M as novel, non-invasive biomarkers to differentiate CD and CU from non-IBD, with promising results,” added Dr. de Meij, who was not involved in the new work but has conducted similar research. “Future research is necessary to establish its potential role in clinical practice, compared to other non-invasive biomarkers like fecal calprotectin.”