Based on his presentation, an autoimmune and vasculitis work-up was initiated. Markers of inflammation were elevated (ESR 40.8 mm/hr, upper limited of normal (ULN)< 10mm/hr, CRP 43, ULN <10mg/L), the ANA and subset serology (including dsDNA, SSA/SSB, RNP, Sm) were negative. Complement levels were normal. Urinalysis was normal with no signs of proteinuria, hematuria or casts. ANCA antibodies came back positive (titer 1:230, Ref < 1.20 AI), with a positive PR3 antibody (titer 5.3, ULN <1.0 AI) and negative MPO-ANCA. Serology for hepatitis B and C and tuberculosis was negative.
A review of the prior emergency department evaluation for his severe headaches revealed a computed tomography (CT) scan of his head that was positive for severe maxillary sinusitis, no acute intracranial hemorrhages/ischemia. A CT of his sinuses confirmed the involvement of the maxillary sinuses bilaterally, but no air fluid levels were noted. The frontal and ethmoidal sinuses were clear, and the ostiomeatal units were unremarkable.
After rheumatology evaluation, treatment with high-dose oral steroids (prednisone 1 mg/kg daily) was initiated and patient was referred back to ENT for sinus biopsy. The pathology report was consistent with granulomatous vasculitis and necrosis involving sinonasal mucosa, revealing extensively inflamed and ulcerated sinonasal tissue with dense lymphoplasmacytic infiltrate and granulation tissue formation. Occasional profiles of medium-size arterioles show infiltration by lymphocytes and occasional giant cells (see Figures 1 and 2).
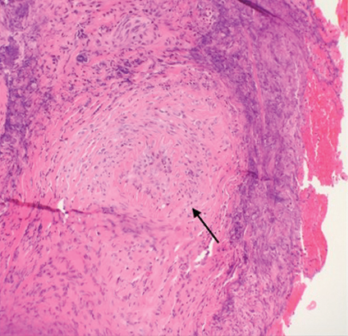
Figure 1. A nasal biopsy shows intimal infiltration of the small blood vessels (black arrow).
To evaluate disease extension, a CT of the chest was obtained. No hilar or mediastinal adenopathy, lung nodules or pleurisy were noted. An audiogram was also performed and was negative for hearing loss.
Based on these data, the disease was considered limited to upper airways. In addition to glucocorticoids, we initiated therapy with oral methotrexate. Clinically, the patient improved quickly. Constitutional symptoms completely resolved, as did the nasal congestion. His ear pain decreased, and his voice improved, along with his appetite and fatigue. Methotrexate was gradually increased over the course of the next three months from 10 mg to 20 mg weekly. The dose of prednisone was gradually tapered over the course of eight months. The patient was also prophylactically treated with trimethoprim/sulfamethoxazole (3x/week), weekly alendronate, daily calcium and vitamin D supplementation.
Three months after GPA diagnosis, his labs noted new-onset microscopic hematuria. A nephrology evaluation was obtained. A kidney biopsy was obtained, and fortunately it was negative for vasculitis changes. Shortly after, the patient was noted to have microscopic kidney stones.

