Over the course of the next year, the patient has experienced complete resolution of virtually all of his symptoms, has been successfully tapered off of prednisone without any recurrence of symptoms and is tolerating methotrexate without any major adverse reactions. He continues to follow up with rheumatology regularly.
Discussion
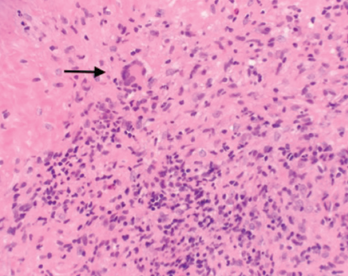
Figure 2. A nasal biopsy shows giant multinuclear cells (black arrow).
GPA is a complex, multisystem disease that is often difficult to diagnose, especially at the initial presentation. Early diagnosis is critical to halt the disease process and progression. Patients with GPA diagnosed early in the disease process, especially in the ambulatory setting, have had favorable outcomes compared with patients enrolled in randomized controlled trials who are usually referred to tertiary centers and present with advanced disease.4 This can certainly be attributed to the delay in diagnosis and or misinterpretation of initial presenting symptoms.
Without increased awareness and proper training to recognize this disease, physicians often omit a vasculitis diagnosis from their differentials. Reported symptoms include, but are not limited to, fatigue, fever, weight loss, arthralgias, rhinosinusitis, cough, voice changes, hearing loss, dyspnea and skin rashes.
Although our patient had a strikingly similar presentation, he was officially diagnosed with GPA eight years after the onset of symptoms. During the five years between the worsening of his symptoms and the diagnosis of GPA, we have been able to track multiple medical visits. Our patient had visited his primary care physician, ENT and infectious disease specialists, as well as made multiple emergency department visits due to recurrent, debilitating symptoms.
A delay in diagnosis can often be fatal. Therefore, establishing a diagnosis early in the disease process is crucial. In 1990, the ACR established criteria to help distinguish GPA from other forms of vasculitis.5 The following criteria were proposed and studied: nasal or oral inflammation (painful or painless oral ulcers, or purulent or bloody nasal discharge), abnormal chest radiograph showing nodules, fixed infiltrates or cavities, abnormal urinary sediment (microscopic hematuria with or without red cell casts) and granulomatous inflammation on biopsy of an artery or perivascular area. The presence of two or more of these four criteria yielded a sensitivity and specificity of 88% and 92% respectively.5 Based on ACR criteria, our patient was diagnosed with GPA.
Once the diagnosis has been suspected clinically, several laboratory markers have been recognized to differentiate GPA from other forms of vasculitis. In 1985, ANCA were linked to GPA.6 Immunofluorescence patterns described in ANCA vasculitis were either diffuse within the cytoplasm (C-ANCA) or perinuclear (P-ANCA).7 Two relevant target antigens, proteinase 3 (PR3) and myeloperoxidase (MPO) located in the azurophilic granules of neutrophils and the peroxidase-positive lysosomes of monocytes were found in ANCA vasculitis. Antibodies that target PR3 and MPO antigens are called PR3-ANCA and MPO-ANCA, respectively.

