Given that multiple differential diagnoses had been ruled out at this point, consideration was given to autoinflammatory disease as a possible diagnosis. The patient was subsequently prescribed 0.6 mg of colchicine twice a day without any improvement.
During this time, the patient developed COVID-19 and started to notice that her periodic episodes were becoming more persistent. Concern for an underlying malignancy prompted evaluation with colonoscopy and computerized tomography (CT) scan of the chest, abdomen and pelvis, which failed to reveal any significant findings apart from a small incidental lung nodule. Further investigation for underlying autoinflammatory disease was eventually performed with Invitae genetic testing.
The genetic panel for autoinflammatory syndromes was positive and heterozygous for a mutation in the NOD2 gene, IVS8+158 and R702W variant. Interestingly, the patient was also found to be positive and heterozygous for a mutation in TNFRSF1A R92Q, the gene associated with TNF receptor-associated periodic syndrome (TRAPS).
Despite having mutations associated with two autoinflammatory disease, the patient was diagnosed with only one autoinflammatory disease, Yao syndrome, based on her clinical presentation. It was decided to start the patient on 150 mg of canakinumab every two months to treat her autoinflammatory disease, to which she had a good response.
Discussion
Diagnosing SAIDs can be an arduous process because the conditions often share identical clinical phenotypes and their presentations often mimic infectious, malignant, allergic and autoimmune disorders, particularly early in the course of disease. A broad differential diagnosis is invariably required and should also include the newly discovered group of autoinflammatory disorders.5,6
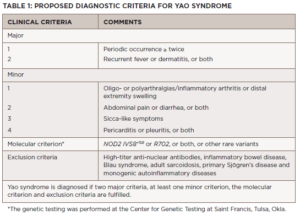
The diagnosis of Yao syndrome requires the presence of clinical criteria, consisting of typical symptoms; molecular criteria, consisting of NOD2 variants; and the proper exclusion of similar diseases, such as inflammatory bowel syndrome, sarcoidosis, Sjögren’s disease, Blau syndrome and other monogenic autoinflammatory syndromes.3,7 The NOD2 variant IVS8+158 is detected in almost all patients with Yao syndrome, with concurrent R702W in up to 30%.3,7
Recently, our growing understanding of the disease has identified even newer genetic variants and other unique manifestations, such as eyelid swelling.8 Table 1 shows the proposed diagnostic criteria for Yao syndrome.9
Differentiating Yao syndrome from other hereditary periodic fever syndromes is an essential part of the diagnostic evaluation.4 Of the autoinflammatory disorders, familial Mediterranean fever (FMF) appears to have the closest phenotypic overlap with Yao syndrome despite having its own distinct genetic mutation in the MEFV gene.